Steal phenomenon from mammary side branches: when does it occur?
-
Upload
sacklerinstitute -
Category
Documents
-
view
0 -
download
0
Transcript of Steal phenomenon from mammary side branches: when does it occur?
1998;66:2056-2062 Ann Thorac SurgPossati
Alessandro Giordano, Carlo Trani, Maria Lucia Calcagni, Paolo Pola and Gianfederico Mario Gaudino, Michele Serricchio, Franco Glieca, Piergiorgio Bruno, Paolo Tondi,
Steal phenomenon from mammary side branches: when does it occur?
http://ats.ctsnetjournals.org/cgi/content/full/66/6/2056on the World Wide Web at:
The online version of this article, along with updated information and services, is located
Print ISSN: 0003-4975; eISSN: 1552-6259. Southern Thoracic Surgical Association. Copyright © 1998 by The Society of Thoracic Surgeons.
is the official journal of The Society of Thoracic Surgeons and theThe Annals of Thoracic Surgery
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
Steal Phenomenon From Mammary Side Branches:When Does It Occur?Mario Gaudino, MD, Michele Serricchio, MD, Franco Glieca, MD,Piergiorgio Bruno, MD, Paolo Tondi, MD, Alessandro Giordano, MD, Carlo Trani, MD,Maria Lucia Calcagni, MD, Paolo Pola, MD, and Gianfederico Possati, MDDepartments of Cardiac Surgery, Angiology, Nuclear Medicine, and Cardiology, Catholic University, Rome, Italy
Background. The hemodynamic significance of patentmammary graft side branches is still controversial. Thisstudy was designed to evaluate the potential for flowsteal of patent mammary side branches in differenthemodynamic conditions.
Methods. Echo-Doppler measurement of mammarygraft flow was performed at rest and after dipyridamole-induced coronary vasodilatation in 10 patients with an-giographic demonstration of evident mammary graft sidebranches (study group) and in 10 matched control pa-tients (control group). Concomitant thallium-201 myocar-dial scintigraphy was performed to assess the adequacyof mammary flow to the myocardial oxygen demand.Patients of the study group were also submitted to flowevaluation in condition of selective muscular or com-bined systemic and coronary relaxation.
Results. No difference in mammary flow and adequacy
to myocardial oxygen demand was detected betweenpatients of the study and control groups both at rest andafter dipyridamole infusion. In patients with patent sidebranches the systolic-to-diastolic flow ratio was main-tained in case of combined coronary and peripheralvasodilatation, whereas selective muscular relaxation ledto an increase in the systolic and a reduction in thediastolic flow.
Conclusions. Flow steal from patent mammary graftside branches is possible only in case of selective mus-cular vasodilatation. As this situation is unlikely to occurin the clinical setting, the potential for flow steal ofmammary side branches in cardiac surgery patientsseems to be minimal.
(Ann Thorac Surg 1998;66:2056–62)© 1998 by The Society of Thoracic Surgeons
The possibility of a steal phenomenon from patentinternal mammary artery (IMA) graft side branches
is still controversial. Although some investigators haveanecdotally reported clinical and instrumental evidenceof myocardial ischemia that regressed after IMA sidebranch embolization or ligature [1–4], angiographic dataand intravascular Doppler studies have minimized thehemodynamic importance of IMA side branches [5–8].Moreover, the published studies have all focused on thepossibility of flow steal at rest or in case of selectivecoronary vasodilatation and no investigation has verifiedthe hemodynamic role of mammary side branches incondition of muscular or combined peripheral and coro-
See also page 1873
nary relaxation (as usually occurs during physicalexercise).
This study protocol was designed to elucidate thehemodynamic role of IMA graft side branches in condi-tion of systemic and coronary vasodilatation by analyzingthe echo-Doppler measurements of mammary flow intwo groups of patients: one with and one without undi-vided IMA graft side branches.
Materials and Methods
Patient PopulationsThis study protocol involved 10 patients with angio-graphic demonstration of evident IMA graft sidebranches (study group) and 10 comparable patients inwhom postoperative angiography revealed an IMA graftwithout side branches (control group).
The 10 components of the study group were selectedamong the 51 patients who underwent minimally inva-sive myocardial revascularization at our departmentfrom January 1995 to December 1996. Patients undergo-ing minimally invasive myocardial revascularization dur-ing this period were chosen because at that time nodedicated chest retractor for minimally invasive proce-dure was available at our institution, therefore, in thesepatients the left IMA was harvested only for a shortlength of its distal tract and all the proximal sidebranches were left patent [9]. All 51 patients underwentpostoperative angiographic control; selection for enroll-ment in this investigation was based on the angiographicdemonstration of normofunctioning left IMA-to-left an-terior descending (LAD) anastomosis with clear evidenceof patent left IMA side branches (at least three proximalside branches with diameter greater than or equal to0.5 mm or a single large branch greater than or equal to1.5 mm in diameter; see Fig 1) and on the willingness of
Accepted for publication June 25, 1998.
Address reprint requests to Dr Gaudino, Divisione di Cardiochirurgia,Policlinico A. Gemelli, Largo A. Gemelli 8, 00168 Rome, Italy.
© 1998 by The Society of Thoracic Surgeons 0003-4975/98/$19.00Published by Elsevier Science Inc PII S0003-4975(98)00979-5
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
the patient to undergo a new scintigraphic and echo-Doppler control.
Patients of the control group were selected among the127 patients with a traditionally performed left IMA-to-LAD anastomosis operated in the same time frame whounderwent postoperative control angiography (due toenrollment in different study protocols) at our institution.At operation in these patients the left IMA was dissecteduntil its origin from the subclavian artery and care waspaid to visualize and interrupt all IMA branches (espe-cially in the proximal tract); for this reason it was judgedthat they could constitute an appropriate control group.Selection for this investigation was based on the angio-graphic demonstration of a normal IMA-to-LAD graft withabsence of angiographically evident IMA side branches,in agreement with the clinical and angiographic charac-teristics of each patient and those of a correspondingpatient of the study group (to obtain two comparableseries; Table 1) and on the willingness of the patient toundergo a new scintigraphic and echo-Doppler control.
A difference of 0.5 mm in the IMA or LAD diameterwas considered acceptable, whereas no difference in LADtype and flow was accepted between a particular mini-mally invasive myocardial revascularization patient andhis or her control. Particular attention was paid to thecorrespondingly paired patient in terms of extension andlocation of previous myocardial infarction, degree of thestenosis on the LAD, ejection fraction, presence of leftventricular hypertrophy, and diabetes mellitus.
Angiographic characteristics of patients of both groupswere measured using a computerized system (CathexCCIP-310 Heart System; Cathex Co, Tokyo, Japan). Allpatients did not take any vasoactive medication for 2 daysbefore each test.
Evaluation of Mammary Artery Flow Reserve andAdequacy to Myocardial Oxygen DemandEcho-Doppler evaluation of mammary artery flow re-serve and adequacy to increased myocardial oxygendemand was performed using a described protocol [10].The following parameters were calculated both at restand after intravenous administration of dipyridamole0.84 mg/kg (Persantin; Boehringer Mannheim, Berlin,Germany): peak systolic velocity (meters per second);end-systolic velocity (meters per second); peak diastolicvelocity (meters per second); end-diastolic velocity(meters per second); time average mean velocity (metersper second); resistance index; pulsatility index; systolic-to-diastolic peak velocity ratio. The time average meanvelocity was defined as the area between the line tracedon the Doppler wave and the baseline. The diameter ofthe IMA was calculated using internal electronic caliperson frozen frame images from the B-mode recording. Flow(F) was obtained using the formula: F (millimeters perminute) 5 time average mean velocity (centimeters per
Fig 1. Postoperative angiographic control in a patient of the studygroup. Patent mammary graft side branches are particularly evident.
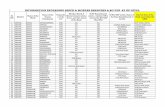
Table 1. Postoperative Angiographic Characteristics of thePatients
PatientNo.
LADDiametera
(mm)
LADTypeb
(I-II-III)LAD Flow(TIMI 0–3)
IMADiameterc
(mm)
IMADiameterd
(mm)
Studygroup1 2.23 III 3 2.72 2.722 2.10 II 3 2.94 2.793 2.33 II 3 2.59 2.174 2.42 III 3 2.78 2.625 2.25 III 3 3.20 2.406 1.93 II 3 2.41 2.357 1.48 II 3 2.71 2.598 1.70 III 2 3.10 2.989 2.42 III 3 2.51 2.5010 2.10 III 3 2.97 2.81
Mean 2.09 6 0.01 2.60 6 0.02 2.90 6 0.01 2.79 6 0.01 2.59 6 0.01Control
group1 2.09 III 3 3.00 2.452 2.12 II 3 2.95 2.803 2.50 II 3 2.40 2.204 2.60 III 3 2.81 2.595 2.00 III 3 3.10 2.606 2.05 II 3 2.50 2.387 1.52 II 3 2.90 2.738 1.90 III 2 2.60 2.479 2.56 III 3 3.20 3.0310 2.81 III 3 2.60 2.55
Mean 2.14 6 0.01 2.55 6 0.02 2.88 6 0.01 2.82 6 0.01 2.58 6 0.01
a Immediately distal to the level of IMA anastomosis. b According tothe CASS classification. c Mean value from the proximal end to themild tract of the IMA. d Mean value in the tract immediately proximalto the anastomosis.
Statistical analysis revealed no difference between the two groups.
IMA 5 internal mammary artery; LAD 5 left anterior descendingartery.
2057Ann Thorac Surg GAUDINO ET AL1998;66:2056–62 IMA SIDE BRANCHES FLOW STEAL
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
second) 3 (pr2 3 60) where r is half the internal diameterof the IMA expressed in centimeters.
Thallium-201 myocardial scintigraphy was performedin all patients immediately after the dipyridamole test.The ischemia index (difference between the scintigraphicscore after dipyridamole infusion and at rest) [10] wasused to quantify the degree of inducible ischemia in theLAD region.
Vasodilatory ProtocolOn a different day the patients of the study group weresubmitted to IMA flow evaluation at rest and in condition
of selective muscular or combined coronary and periph-eral vasodilatation.
Muscular vasodilatation was achieved in 7 patients bythe intravenous administration of 500 mg of xantinolenicotinate (Complamin; Italchimici, Rome, Italy), an al-most selective peripheral vasodilator widely used inEurope to increase blood flow to ischemic muscles in caseof peripheral arterial disease [11]. After xantinole nicoti-nate infusion the patients were kept supine and immo-bile and the heart rate was continuously monitored for 15minutes to identify and exclude patients in whom theadministration of this drug led to excessive reflex tachy-cardia (defined as an increase of more than 10 beats perminute of the baseline frequency) with consequent cor-onary vasodilatation (an event that occurred in 2patients).
Combined coronary and systemic vasodilatation wasobtained in 10 patients using either 20 mg of sublingualnifedipine (Adalat; Bayer, Hamburg, Germany) or forcedventilation for 2 minutes (which was supposed to in-crease the flow in the intercostal muscles served by theIMA and to induce reflex tachycardia and coronaryrelaxation).
Statistical AnalysisData are expressed as mean 6 standard deviation. Theunpaired Student’s t test was used to compare the hemo-dynamic characteristics of IMA flow at rest and aftersystemic or coronary vasodilatation. Two-factor analysisof variance for repeated measures was used to evaluatedifferences between the study and control groups and thedifferent vasodilator agents. Post hoc comparison withNewman-Keuls test was used to analyze single factors. Ap value less than 0.05 was considered significant.
Results
Dipyridamole TestDetailed results of the echo-Doppler measurement atrest and after dipyridamole infusion in the two groups
Fig 2. Echo-Doppler evaluation of left internal mammary arteryflow at rest (A) and after diypyridamole infusion (B) in a patient ofthe study group. Increase in diastolic peak velocity (V3) is superiorto increase in systolic peak velocity (V1). (V2 5 end-systolic veloc-ity, V4 5 end-diastolic velocity.)
Table 2. Left Internal Mammary Artery Flow Characteristics at Rest and After Dipyridamole Infusion in the Two Groups
At Rest VersusDipyridamole
Study Group
PSV(m/s)
ESV(m/s)
PDV(m/s)
EDV(m/s)
TAMV(m/s) PI RI SDR
Flow(mL/min)
Diameter(mm)
Rest 0.33 6 0.07 0.06 6 0.04 0.26 6 0.12 0.14 6 0.07 0.18 6 0.06 2.01 6 1.11 0.89 6 0.14 1.24 6 0.40 67.8 6 22.6 2.95 6 0.24Dipyridamole 0.43 6 0.17 0.22a 6 0.08 0.67a 6 0.22 0.38a 6 0.18 0.40 a6 0.14 0.55a 6 0.31 0.82 6 0.15 0.68a 6 0.23 150.7a 6 52.7 3.09 6 0.25
Table 3. Scintigraphic Results
GroupDyp–SPET
(mean score)Rest–SPET
(mean score) Ischemia Index
Study 0.90 0.70 0.20Control 1.50 6 3.17 1.20 6 2.57 0.30 6 0.67
Dyp 5 dipyridamole; SPET 5 single photon emission tomography.
Statistical analysis revealed no difference between the two groups.
2058 GAUDINO ET AL Ann Thorac SurgIMA SIDE BRANCHES FLOW STEAL 1998;66:2056–62
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
are shown in Table 2. No statistical difference in peaksystolic velocity, peak diastolic velocity, and flow wasfound between the study and control groups at rest andafter dipyridamole administration. In both groups IMAflow after dipyridamole infusion was significantly supe-rior than at baseline (p , 0.01 for both) with the maximalincrease recorded in the peak diastolic velocity (Fig 2).
No significant difference in the amount of inducibleischemia in the LAD region could be demonstratedamong study and control patients. Only 1 patient of thestudy group and 2 patients of the control group showedminor perfusion deficit in the LAD region (Table 3); in all3 patients a nongrafted anterolateral or diagonal branchwas considered responsible for the scintigraphically de-tected ischemia in the anterior region.
Selective Muscular VasodilatationXantinole nicotinate infusion led to a small increase ofthe IMA flow. This flow increase was the result of anincrease in the systolic and a small reduction in thediastolic component of the IMA flow (expressed by anincrease in the peak systolic velocity, a decrease in thepeak diastolic velocity, and an increase in the systolic-to-diastolic peak velocity ratio) (Table 4).
Combined Systemic and Coronary VasodilatationForced ventilation and nifedipine led to an increase ofboth systolic and diastolic flow; in both cases the diastoliccomponent increased slightly more than the systoliccomponent, leading to a reduction of the systolic-to-diastolic peak velocity ratio (Tables 5 and 6, respectively).
Comment
The hemodynamic importance of patent mammary ar-tery side branches and their possible effect on IMA graft
function are still controversial. Angina recurrence hasanedoctally been reported in patients who received anIMA graft and in whom patent IMA side branches(pericardiophrenic or intercostal) were particularly evi-dent [1–4]. In most patients, clinical and instrumentalevidence of myocardial ischemia disappeared after inter-ruption (either surgical or percutaneous) of IMA sidebranches, supporting the hypothesis of a significant de-viation of mammary blood flow through them.
On the other hand, patent IMA side branches consti-tute a quite common finding at postoperative angiogra-phy and their association with reduced coronary perfu-sion or IMA malfunction has been denied in at least twolarge angiographic studies [5, 6]. Moreover, Kern andcolleagues [7], using an intravascular Doppler-tippedflowmeter inserted in an IMA graft and in a largepectoralis branch, demonstrated minimal flow diversionin the side branch either at rest and during adenosine-induced coronary hyperemia. More recently Luise andcoworkers [8] using a similar technique demonstratedlack of significant difference in the flow characteristicsbetween patients with and without patent IMA graft sidebranches at rest and after intracoronary adenosineinfusion.
However, none of the published studies investigatedthe possibility of flow steal from the IMA branches incondition of peripheral (or combined systemic and coro-nary) vasodilatation. If the possibility of blood steal fromthe IMA side branches exists, it seems conceivable thatflow diversion occurs in condition of systemic (and notcoronary) relaxation. Instead, the intracoronary infusionof adenosine produces a selective amelioration of IMAcoronary run-off, nonphysiologically increasing the dif-ference between the high resistance muscular and thelow resistance coronary beds and thus minimizing thepossibility of flow steal from the side branches.
Table 4. Left Internal Mammary Artery Flow Characteristics in the Patients of the Study Group After Xantinole NicotinateAdministration
Rest VersusXantinoleNicotinate
PSV(m/s)
ESV(m/s)
PDV(m/s)
EDV(m/s)
TAMV(m/s) PI RI SDR
Flow(mL/min)
Diameter(mm)
Rest 0.32 6 0.08 0.07 6 0.05 0.28 6 0.15 0.15 6 0.01 0.21 6 0.04 1.24 6 0.52 0.93 6 0.04 1.14 6 0.42 79.1 6 15.0 2.90 6 0.23Xantinole
nicotinate0.34 6 0.14 0.07 6 0.02 0.25 6 0.13 0.13 6 0.07 0.20 6 0.07 1.64 6 0.42 0.95 6 0.02 1.36 6 0.46 84.7 6 29.1 3.00 6 0.25
EDV 5 end-diastolic velocity; ESV 5 end-systolic velocity; PDV 5 peak diastolic velocity; PI 5 pulsatility index; PSV 5 peak systolicvelocity; RI 5 resistance index; SDR 5 systolic–diastolic peak velocity ratio; TAMV 5 time average mean velocity.
Table 2. Continued
Control Group
PSV(m/s)
ESV(m/s)
PDV(m/s)
EDV(m/s)
TAMV(m/s) PI RI SDR
Flow(mL/min)
Diameter(mm)
0.33 6 0.12 0.06 6 0.04 0.27 6 0.04 0.14 6 0.04 0.19 6 0.05 2.00 6 0.96 0.90 6 0.09 1.45 6 0.63 71.5 6 18.8 2.94 6 0.330.43 6 0.10 0.22a 6 0.07 0.67a 6 0.19 0.40a 6 0.16 0.39a 6 0.12 0.55a 6 0.31 0.82 6 0.10 0.63a 6 0.16 146.9a 6 45.2 3.10 6 0.35
a p #0.01 compared with baseline. Statistical analysis revealed no significant differences between the two groups in any condition.
EDV 5 end-diastolic velocity; ESV 5 end-systolic velocity; PDV 5 peak diastolic velocity; PI 5 pulsatility index; PSV 5 peak systolicvelocity; RI 5 resistance index; SDR 5 systolic–diastolic peak velocity ratio; TAMV 5 time average mean velocity.
2059Ann Thorac Surg GAUDINO ET AL1998;66:2056–62 IMA SIDE BRANCHES FLOW STEAL
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
The use of transthoracic echo-Doppler for the assess-ment of IMA patency is widely accepted in clinicalpractice [12, 13]. The recent validation of this method forthe study of IMA flow variations in response to vasoac-tive substances or in stress conditions [14, 15] led us tochoose this technique for the investigation of the IMA-to-side branches steal phenomenon.
In our series no difference in left IMA flow was de-tected between patients with and without patent IMAbranches either at rest and after dipyridamole-inducedcoronary vasodilatation. The increase in IMA flow wasalways able to meet the myocardial oxygen demand andno scintigraphically evident flow steal could be demon-strated in patients of the study group.
Assuming that in the left IMA of patients of the studygroup systolic blood flow is mainly directed to the sidebranches and diastolic flow is essentially to the LAD, ashypothesized by Kern and coworkers [7], it is possible toextrapolate from our data the relative hemodynamicimportance of IMA branches and LAD vascular bed indifferent conditions.
Fig 3. Echo-Doppler evaluation of left internal mammary arteryflow at rest (A) and after 2 minutes of forced ventilation (B) in apatient of the study group. There is an increase in both the peaksystolic velocity (V1) and the peak diastolic velocity (V3). (V2 5end-systolic velocity, V4 5 end-diastolic velocity.)
Tabl
e5.
Left
Inte
rnal
Mam
mar
yA
rter
yFl
owC
hara
cter
istic
sin
the
Patie
nts
ofth
eSt
udy
Gro
upA
fter
2M
inut
esof
Forc
edV
entil
atio
n
Res
tvs
Forc
edV
enti
lati
onP
SV(m
/s)
ESV
(m/s
)P
DV
(m/s
)E
DV
(m/s
)T
AM
V(m
/s)
PI
RI
SDR
Flow
(mL
/min
)D
iam
eter
(mm
)
Res
t0.
376
0.03
0.08
60.
040.
316
0.12
0.07
60.
030.
206
0.04
1.50
60.
520.
916
0.04
1.19
60.
4475
.36
15.0
2.85
60.
58
Forc
ed
ven
tila
tion
0.41
60.
120.
12a
60.
020.
396
0.09
0.18
a6
0.05
0.25
a6
0.04
1.36
60.
260.
96a
60.
011.
056
0.30
94.2
a6
15.6
3.05
60.
56
ap
#0.
01co
mp
ared
wit
hba
selin
e.
ED
V5
end
-dia
stol
icve
loci
ty;
ESV
5en
d-s
ysto
licve
loci
ty;
PD
V5
pea
kd
iast
olic
velo
city
;P
I5
pu
lsat
ility
ind
ex;
PSV
5p
eak
syst
olic
velo
city
;R
I5
resi
stan
cein
dex
;SD
R5
syst
olic
–d
iast
olic
pea
kve
loci
tyra
tio;
TA
MV
5ti
me
aver
age
mea
nve
loci
ty.
2060 GAUDINO ET AL Ann Thorac SurgIMA SIDE BRANCHES FLOW STEAL 1998;66:2056–62
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
At rest most of the IMA graft flow occurs in diastole;this systolic-to-diastolic flow ratio obviously decreases incondition of selective coronary relaxation (Fig 2) andremains almost unchanged in case of simultaneous cor-onary and systemic vasodilatation (as is in the case ofnifedipine administration or forced ventilation) (Figs 3and 4).
Instead, the administration of a pure muscular vasodi-lator (xantinole nicotinate) leads to a reduction of thediastolic and an increase in the systolic component ofIMA flow (Fig 5), allowing the hypothesis of a flow stealfrom the dilated side branches. However, as in physio-logic conditions systemic vasodilatation is usually accom-panied by coronary relaxation (direct of reflex), this typeof blood steal seems unlikely to occur in the clinicalsetting.
Although this study is based on a limited number ofobservations, the accuracy of the patient selection andthe reproducibility of the echo-Doppler results are strongarguments in favor of the validity of our methodologyand the applicability of our results to the great majority ofpatients submitted to coronary artery bypass grafting.
Fig 4. Echo-Doppler evaluation of left internal mammary arteryflow at rest (A) and after nifedipine administration (B) in a patientof the study group. There is an increase in both the peak systolicvelocity (V1) and the peak diastolic velocity (V3). (V2 5 end-systolic velocity, V4 5 end-diastolic velocity.)Ta
ble
6.Le
ftIn
tern
alM
amm
ary
Art
ery
Flow
Cha
ract
eris
tics
inth
ePa
tient
sof
the
Stud
yG
roup
Aft
erN
ifed
ipin
eA
dmin
istr
atio
n
Res
tvs
Nif
edip
ine
PSV
(m/s
)E
SV(m
/s)
PD
V(m
/s)
ED
V(m
/s)
TA
MV
(m/s
)P
IR
ISD
RFl
ow(m
L/m
in)
Dia
met
er(m
m)
Res
t0.
336
0.03
0.10
60.
030.
266
0.10
0.13
60.
010.
196
0.05
1.43
60.
610.
936
0.02
1.26
60.
4165
.26
9.4
2.20
60.
61
Nif
edip
ine
0.37
60.
090.
106
0.03
0.31
60.
070.
126
0.03
0.23
60.
011.
706
0.31
0.97
a6
0.01
1.19
60.
3386
.6a
65.
72.
406
0.55
ap
#0.
01co
mp
ared
wit
hba
selin
e.
ED
V5
end
-dia
stol
icve
loci
ty;
ESV
5en
d-s
ysto
licve
loci
ty;
PD
V5
pea
kd
iast
olic
velo
city
;P
I5
pu
lsat
ility
ind
ex;
PSV
5p
eak
syst
olic
velo
city
;R
I5
resi
stan
cein
dex
;SD
R5
syst
olic
–d
iast
olic
pea
kve
loci
tyra
tio;
TA
MV
5ti
me
aver
age
mea
nve
loci
ty.
2061Ann Thorac Surg GAUDINO ET AL1998;66:2056–62 IMA SIDE BRANCHES FLOW STEAL
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
On the basis of the reported observations it is ourimpression that, when the IMA-to-coronary artery anas-tomosis is well constructed and the coronary artery has agood caliber and length, diversion of blood flow from thecoronary system to the side branches is a remote possi-bility. However, if technical imperfections (anastomoticstenosis) or anatomic factors (small quality and diameterof the distal IMA or the target vessel) reduce the IMArun-off, flow can probably be diverted into large sidebranches with lower resistance.
In support of this theory, in at least two of the pub-lished cases of flow steal an anastomotic stenosis wasassociated with the persistence of mammary sidebranches [4, 16]; in both patients clinical improvementand increase of IMA diameter were achieved after per-cutaneous dilatation of the anastomosis, even in theabsence of complete side branch occlusion. It is conceiv-able that in these patients the resolution of the anasto-motic stenosis has led to a significant amelioration of theIMA run-off, restoring the normal ratio between mam-mary graft and side branch resistances and thus, mini-mizing flow diversion in the IMA branches.
In conclusion, our data suggest that, although a mini-mal flow steal is observable in case of selective muscularvasodilatation, mammary flow diversion in the sidebranches can occur only to a minimal extent in physio-logic conditions. The IMA flow steal from patent sidebranches is probably the result of a rare combination ofunfavorable anatomic and technical conditions, with lim-ited impact in the general population of patients under-going coronary operations.
References
1. Schmid C, Heublein B, Reichelt S, Borst HG. Steal phenom-enon caused by a parallel branch of the internal mammaryartery. Ann Thorac Surg 1990;50:463–4.
2. Nakhjavan FK, Koolpe HA, Bruss J, Najhi M, Radke T.Transcatheter coil occlusion for treatment of left internalmammary–anterior descending artery steal phenomenon.Cathet Cardiovasc Diagn 1993;28:347–50.
3. Ayres RW, Lu CT, Benzuly KH, Hill GA, Rossen JD. Trans-catheter embolization of an internal mammary artery bypassgraft sidebranch causing coronary steal syndrome. CathetCardiovasc Diagn 1994;31:301–3.
4. Mishkel GJ, Willinsky R. Combined PTCA and microcoilembolization of a left internal mammary artery graft. CathetCardiovasc Diagn 1992;27:141–6.
5. Ivert T, Huttunen K, Landou C, Bjork VO. Angiographicstudies of the internal mammary artery 11 years after coro-nary artery bypass grafting. J Thorac Cardiovasc Surg 1988;96:1–12.
6. Kuttler H, Hauenstein KH, Wenz W, Schlosser V. Signifi-cance of early angiographic follow-up after internal thoracicartery anastomosis in coronary surgery. Thorac CardiovascSurg 1988;36:96–9.
7. Kern MJ, Bach RG, Donohue TJ, Caracciolo EA, Wolford T,Aguirre FV. Role of large pectoralis branch artery in flowthrough a patent left internal mammary artery conduit.Cathet Cardiovasc Diagn 1995;34:240–4.
8. Luise R, Teodori G, Di Gianmarco G, et al. Persistence ofmammary artery branches and blood supply to the leftanterior descending. Ann Thorac Surg 1997;63:1759–64.
9. Possati G, Gaudino M, Alessandrini F, Zimarino M, Glieca F,Luciani N. Systematic clinical and angiographic follow-up ofpatients submitted to minimally invasive coronary arterybypass. J Thorac Cardiovasc Surg 1998;115:785–90.
10. Gaudino M, Serricchio M, Tondi P, et al. Non-invasiveevaluation of mammary artery flow reserve and adequacy toincreased myocardial oxygen demand. Eur J CardiothoracicSurgery 1998;13:404–9.
11. Reynolds JEF, ed. Martindale the extrapharmacopeia. Lon-don: The Pharmaceutical Press, 1993.
12. Van Son JAM, Skotnicki SH, Peters MBM, Pijls NHJ, NoyezL, van Asten WNJC. Noninvasive hemodynamic assessmentof the internal mammary artery in myocardial revasculariza-tion. Ann Thorac Surg 1993;55:404–9.
13. Canver CC, Armstrong VM, Nichols RD, Mentzer RM.Color-flow duplex ultrasound assessment of internal tho-racic artery graft after coronary bypass. Ann Thorac Surg1995;59:389–92.
14. Takemura H, Kawasuji M, Sakakibara N, Tedoriya T, Ushi-jima T, Watanabe Y. Internal thoracic artery graft functionduring exercise assessed by transthoracic Doppler echogra-phy. Ann Thorac Surg 1996;61:914–9.
15. Canver CC, Armstrong VM, Cooler SD, Nichols RD. Assess-ment of internal thoracic artery vasoreactivity in response tosublingual nitroglycerin. Ann Thorac Surg 1997;63:1041–3.
16. Ishizaka N, Ikari Y, Saeki F, et al. Repeat embolization of theside branch of the internal mammary artery graft by gelatinsponge particles and micro coils. Cathet Cardiovasc Diagno-sis 1995;34:245–9.
Fig 5. Echo-Doppler evaluation of left internal mammary arteryflow at rest (A) and after xantinole nicotinate infusion (B) in a pa-tient of the study group. There is an increase in the peak systolicvelocity (V1) and a decrease in peak diastolic velocity (V3). (V2 5end-systolic velocity, V4 5 end-diastolic velocity.)
2062 GAUDINO ET AL Ann Thorac SurgIMA SIDE BRANCHES FLOW STEAL 1998;66:2056–62
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from
1998;66:2056-2062 Ann Thorac SurgPossati
Alessandro Giordano, Carlo Trani, Maria Lucia Calcagni, Paolo Pola and Gianfederico Mario Gaudino, Michele Serricchio, Franco Glieca, Piergiorgio Bruno, Paolo Tondi,
Steal phenomenon from mammary side branches: when does it occur?
& ServicesUpdated Information
http://ats.ctsnetjournals.org/cgi/content/full/66/6/2056including high-resolution figures, can be found at:
References http://ats.ctsnetjournals.org/cgi/content/full/66/6/2056#BIBL
This article cites 14 articles, 8 of which you can access for free at:
Citationshttp://ats.ctsnetjournals.org/cgi/content/full/66/6/2056#otherarticlesThis article has been cited by 10 HighWire-hosted articles:
Permissions & Licensing
[email protected]: orhttp://www.us.elsevierhealth.com/Licensing/permissions.jsp
in its entirety should be submitted to: Requests about reproducing this article in parts (figures, tables) or
Reprints [email protected]
For information about ordering reprints, please email:
by on June 2, 2013 ats.ctsnetjournals.orgDownloaded from