Silk fibroin/poly(carbonate)-urethane as a substrate for cell growth: in vitro interactions with...
-
Upload
independent -
Category
Documents
-
view
9 -
download
0
Transcript of Silk fibroin/poly(carbonate)-urethane as a substrate for cell growth: in vitro interactions with...
Biomaterials 24 (2003) 789–799
Silk fibroin/poly(carbonate)-urethane as a substrate for cell growth:in vitro interactions with human cells
Anna Chiarinia,*, Paola Petrinib, Sabrina Bozzinib, Ilaria Dal Praa, Ubaldo Armatoa
aDepartment of Biomedical & Surgical Sciences, Histology & Embryology Unit, Verona, ItalybLaboratory of Biomaterials, Department of Bioengineering, Politecnico di Milano, Milan, Italy
Received 1 May 2002; accepted 6 September 2002
Abstract
Silk fibroin (SF)-based or -coated biomaterials are likely to be endowed with structural and surface properties that render them
particularly apt for biomedical applications. In this work we investigated the behavior of four different strains of normal human
adult fibroblasts that had been seeded onto membranes made up of poly(carbonate) urethane (PCU), the surfaces of which had or
had not been homogeneously coated with SF. Cell adhesion within 3 h to the SF-coated PCU films was 2.2-fold that to their
uncoated homologues. After 30 days of incubation in vitro, 2.5-fold more cells had grown on the SF-coated specimens than on the
uncoated ones. This enhanced cell adherence and hence growth on the SF-coated surfaces was coupled with higher cumulative rates
of d-glucose (but not l-glutamine) uptake and of both lactate and interleukin-6 (IL-6) cumulative secretion. Conversely, human
fibroblasts cultured on either type of PCU scaffolds never secreted any ELISA-assayable amount of three main proinflammatory
cytokines, namely interleukin-1b (IL-1b), tumor necrosis factor-a (TNF-a), and transforming growth factor-b1 (TGF-b1). Finally,when the metabolic activities were compared on a per 105 cells basis, it became clear that the adhesion to SF favored an initially
higher consumption of d-glucose, a late higher release of IL-6, and an at-first more intense, but declining, extracellular assembly of
type I collagen fibers. Overall, these results show that SF-coated PCU membranes represent a novel type of biomaterial that favors
the adhesion, the growth and performance of specific metabolic tasks by normal human adult fibroblasts without eliciting any
concurrent secretion of some of the chief proinflammatory cytokines.
r 2002 Elsevier Science Ltd. All rights reserved.
Keywords: Silk fibroin; Poly(carbonate) urethanes; Human fibroblasts; Cytocompatibility; Proinflammatory cytokines
1. Introduction
Raw silk fibers are composed of inner filaments of aprotein, fibroin, embedded in an outer rubbery coatingmade up by another protein species, i.e. sericin. Silkfibroin (SF) is a linear polypeptide, whose maincomponents, i.e. glycine and alanine, are nonpolaramino acids [1]. Silk threads were used as such forsurgical sutures until sensitization to sericin of thepatients submitted to repeat surgical procedures wasreported [2]. Conversely, surgical sutures performed
with degummed, i.e. sericin-deprived, silk fibers werefound to be unable to induce sensitization responses inhumans [2]. In addition, the results of in vivo experi-ments showed that regenerated SF had no thrombo-genicity [3], while in vitro studies revealed that SF filmscould support the adhesion and growth of rodentfibroblasts [1,4–7] and that SF had no significantinflammatory properties [8]. Considering this ability topromote cell adhesion, SF has been the object ofincreasing interest as a potential biomaterial apt fortissue regeneration and repair [1].The possibility of conjugating the peculiar biocom-
patibility of SF with properties typical of differentpolymeric materials (e.g. mechanical properties, biode-gradation/biostability, porosity) is particularly attrac-tive. Recent papers described fibroin-based materials,mainly SF/polymer combinations with polyester [9],sodium alginate [10], polyvinyl alcohol [11], chitosan[12], and acrylic compounds [13]. Surface grafting of SF
Abbreviations: EtOx, ethylene oxide; HUVEC, human umbilical vein
endothelial cells; IL-1b, interleukin-1b; IL-6, interleukin-6; MeOH,
methanol; PCU, poly(carbonate) urethane; PST, poly(styrene); SF, silk
fibroin; TGF-b1, transforming growth factor-b1; TNF-a, tumor
necrosis factor-a.*Corresponding author. Tel.: +39-045-802-7159; fax: +39-045-802-
7159.
E-mail address: [email protected] (A. Chiarini).
0142-9612/02/$ - see front matter r 2002 Elsevier Science Ltd. All rights reserved.
PII: S 0 1 4 2 - 9 6 1 2 ( 0 2 ) 0 0 4 1 7 - 9
was reported onto poly(d,l-lactic acid) [14,15]. Moreover,silk fibroin was modified to favorably alter its chemical–physical properties [16] and promote bone formation [17].The possibility of modifying the surface of polyur-
ethanes—in particular, a medical grade commercialpoly(carbonate)-urethane (Bionate)—with silk fibroinand the chemical–physical characterization of the sub-strates thus obtained was reported in a previous paper [18].Bionate is a commercial medical grade poly(carbo-
nate)-urethane (PCU), developed in alternative topolyether-urethanes for long-term implants. Several invitro and animal studies have shown that Bionate and,in general, PCUs exhibit a superior biostability [19–21].The biocompatibility of polyurethanes, and poly(carbo-nate)-urethanes, is widely accepted and extensivelytested. Notwithstanding this, cytotoxic effects of Bio-nate on human umbilical endothelial cells (HUVEC)were previously reported [22]. However, PCUs bythemselves do not possess surface properties aimed atpromoting cell adhesion and specific protein absorption[22–24], unless surface modifications are induced[25–28]. Anyway, in some cases surface modificationscan be time-consuming and, hence, pricey compared tothe conventional and well-established forthright proces-sing of polymers.Conceivably, novel substrates composed of a film of
Bionate and a homogeneous coating of SF would beendowed with surface characteristics fairly adequate forhuman cell adhesion and growth. Moreover, such an SFcoating would elicit specific changes in cellular behaviorand metabolism as the conformation of a protein on thesurface of a material is deeply affected by the surfacechemistry of the latter. So far, no data concerning thecellular responses to these PCU+SF substrates [18] hadbeen reported.Therefore, the aim of this work was to explore the
interactions between normal adult human fibroblastsand substrates composed by a film of Bionate coatedwith SF. In particular, the effects on cell adhesion, cellgrowth, consumption of metabolic fuels, release ofcatabolites, extracellular assembly of collagen fibers,and proinflammatory cytokine secretion were investi-gated, as altogether these parameters reveal fundamentalfacets of the interactions taking place between human cellsand biomaterials. The results to be reported in this papershow that SF-coated medical grade PCU membranes areendowed with a significantly enhanced biocompatibilitywith respect to the normal adult human fibroblast.
2. Experimental
2.1. Regeneration of silk fibroin
Bombyx mori silk twill 2/2 fabric (Ratti S.p.A., Como,Italy) was soaked in 9.3m LiBr at 601C for 30min [6].
The suspension thus obtained was filtered and thor-oughly dialyzed against distilled water using SpectraPormembrane tubing (MWCO 3500, Bio-Rad Laboratories,Inc., Hercules, CA). The concentrations of the resultingsolutions were calculated from the dry weight of 1.0 g ofSF solution.
2.2. PCU film preparation
PCU films (thickness 0.4mm) were obtained bysolvent casting from a 15% THF:Diox (2:1) solutionof medical grade Bionate 80A (lot number 092696,Polymer Technology Group, CA, USA) at roomtemperature until steady weight was reached (48 hdrying).
2.3. Preparation of 2D SF-coated PCU substrates
Films were cut into rectangular specimens(26� 33mm) to precisely cover the bottom of the wellsof poly(styrene) (PST) eight-well multidish plates withlids (#176600; Nalge Nunc International, IL, USA). Bymeans of a paraffin compound (Bio-Plast Plus, cod. 08-7920, Bio-Optica, Milan, Italy), previously melted at601C, films were stuck to the well bottoms forsubsequent cell culture experiments. This avoided boththe floating of the films in the growth medium and thedischarge of the cells from the surface of the substrates.Such a treatment did not interfere at all with thesuccessive sterilization of the samples and exerted nocytotoxic effect whatsoever on the cultured cells.PCU films were coated with an SF film by immersing
them into freshly prepared SF aqueous solutions.Samples were dried at room temperature until steadyweight, then treated with methanol (MeOH) and driedat room temperature. The amount of SF adhering to thesurface was evaluated from the dry weight of thesubstrates. Uncoated PCU substrates were prepared inparallel as direct controls. Both SF-coated and uncoatedPCU substrates underwent very thorough washing withseveral changes of distilled water a day for a week beforebeing used for human cell cultures.
2.4. Substrates sterilization
The SF-coated PCU membranes were sterilized byexposing them to ethylene oxide (EtOx) gas according tostandard hospital protocols as we had previously foundthat, at variance with ethanol and ethylether, EtOx doesnot induce any appreciable change in the physico-chemical properties of SF membranes [29]. Briefly, oncesealed in sterilization pouches, specimens were exposedfor 3 h at 551C to a mixture of EtOx/CO2 (10/90 v/v)under a pressure of 42 psi. Thereafter, the samplesunderwent 24 h aeration at room temperature and afurther 8 h degassing at 501C in a vacuum oven.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799790
2.5. SF-coating stability
To evaluate the stability of the SF coatings understatic flow conditions, SF-coated PCU substrates,treated with MeOH, were immersed into phosphatebuffer saline (PBS, pH 7.4) and kept at 371C for timelags ranging from 6h to 14 days [18]. Bacterial growthwas prevented by adding sodium azide (0.01%w/v) tothe PBS. PBS extracts were next analyzed by UV and theconcentration of the released SF was determined bymeans of a protein microassay kit (Bio-Rad) usingBradford’s dye-binding procedure (see [18] for details).Moreover, a set of SF solutions of known decreasingconcentrations (from 460 to 5.0 mg/ml) was used toconstruct a proper standard curve for the SF proteinassay [18].
2.6. SEM
Specimens mounted onto aluminum stubs weresputter-coated with gold and next examined in a LeicaCambridge Stereoscan 360 microscope at an accelera-tion voltage of 3–7 kV.
2.7. Cell cultures
Four strains of normal adult fibroblasts were used.Cells were previously isolated from skin biopsies taken,after informed consent, from as many healthy humanvolunteers, next expanded at 371C in vitro, and finallykept stored at –1961C in liquid nitrogen. When required,cell vials were quickly thawed, and the percent fractionof viable cells was assessed under an IM35 Zeiss invertedfluorescence microscope using a Live/Deads Viability/Cytotoxicity kit according to the manufacturer’s in-structions (Molecular Probes, Inc., Eugene, OR). Cellnumbers were next determined by hemocytometercounts, and 1.0� 106 living fibroblasts were initiallyseeded into each of the several polystyrene F–160 flasks(Costar srl, Milan, Italy) to be incubated at 371C inDulbecco’s modified Eagle’s minimum essential medium(DMEM, 90% v/v; Sigma Chemical Co., St. Louis,MO), fortified with inactivated (at 561C for 30min) fetalbovine serum (5% v/v; Biowhittaker Italia srl, Milan,Italy), and antibiotics (sodium penicillin 200 UI/ml;streptomycin 200 mg/ml; amphotericin B 0.5 mg/ml). Thisstandard growth medium was also used for all theexperiments carried out for the present work. Prior toreaching full confluence, the cells were detached fromthe flasks’ surfaces by way of a slight treatment with anEGTA (200mg/l)/trypsin 1:250 (500mg/l) solutiondiluted 1:5 (v/v) in PBS, and their total numbers andviable fractions were determined as just described.Finally, 1.0� 105 fibroblasts were seeded onto eachsample of the previously sterilized SF-coated or un-coated PCU membranes (11,700 cells/cm2) stuck to
eight-well PST plates (Nalge Nunc International).Thereafter, cell morphology was periodically checkedunder the microscope by means of phase contrast orfluorescence optics (in the latter instance after intravitallystaining the cells with a lipophilic fluorescent tracer: seebelow). Cell-conditioned growth media were changedwith fresh ones every 4 days and samples of the cell-conditioned media were stored at –801C to be subse-quently analyzed by biochemical means. Each experimentwas performed at least four times (N ¼ 8 wells/group).
2.8. Cell adhesion and proliferation
To assess the attachment of human cells to uncoatedor SF-coated PCU membranes, prior to plating, humanfibroblasts were intravitally labeled with DiI (DiIC18), afluorescent long-chain lipophilic carbocyanine tracer(Molecular Probes, Inc.) according to the manufac-turer’s instructions. Notably, once incorporated into cellmembranes, such tracers do not interfere with normalcell functioning, thereby allowing a long-term recogni-tion of the labeled cells. DiI gives out an intense orangefluorescence visible with standard rhodamine opticalfilters. Micrographs were taken using an Olympus C-3300 camera, downloaded to a personal computer andworked upon with Adobe Photoshopt, version 5.5software.At 3 h after seeding as well as at the several incubation
times considered, the numbers of cells adhering to thesubstrates were indirectly estimated by means of thecellular uptake of crystal violet stain according to Gotohet al. [5]. Parallel evaluations were also carried out bymeans of a modified Alamar bluet assay (Serotec Ltd.,Kidlington, Oxford, UK). The results gained out of thetwo methods were found to be superimposable. Stan-dard absorbance curves for either of the cell countingmethod were constructed by using cultures onpoly(styrene) flasks, whose varying degrees of cellcrowding had been directly estimated under the phasecontrast microscope (see [30] for details). Each experimentwas performed at least four times (N ¼ 8 wells/group).
2.9. Cell metabolism
The cellular utilization of d-glucose was appraised inthe cell-conditioned growth medium samples by aglucose oxidase assay according to Trinder et al. [31],as developed by Sigma (St. Louis, MO, USA). Therelease of lactic acid into the cell-conditioned growthmedium samples was assessed via a lactate oxidase assayaccording to Barham et al. [32], again as developed bySigma. The cellular uptake of l-glutamine was evaluatedas follows: 20 ml of each conditioned growth mediumsample was incubated for 15min at 371C with 0.1msodium acetate, pH 4.9, in the presence of 0.05 unitsof glutaminase (EC 3.5.1.2) to convert the l-glutamine
A. Chiarini et al. / Biomaterials 24 (2003) 789–799 791
into glutamate and ammonium (NH3). The resultingamount of ammonium was next determined by thereductive amination of 3.4mm 2-oxoglutarate, using 12units of l-glutamate dehydrogenase (GLDH) and0.23mm reduced NADPH in 0.1m sodium phosphate,pH 7.4. Finally, the decrease in absorbance at 340 nm,due to the oxidation of NADPH, was quantified, and itwas proportional to the concentration of the l-glutamine remaining in the cell-conditioned mediumsamples. In each of the above instances as well as in thecase of IL-6 secretion (see below), cumulative curveswere constructed from the data pertaining to cellsattached to SF-coated or uncoated PCU substrates,and the values were normalized taking as equal to one asthe mean value at day 4 of incubation in vitro.Moreover, to compare in relation with time the effectsexerted by either kind of substrate, the metabolicactivities of 105 fibroblasts grown on SF-coated oruncoated PCU films were matched up at correspondingtime points. Each experiment was performed at leastfour times (N ¼ 8 wells/group).
2.10. ELISA assay of proinflammatory cytokines
released into the growth medium
To assess the fibroblastic secretion of variouscytokines into the growth medium with either biomate-rial tested, we employed various commercial ELISA kitsfollowing the instructions of the manufacturers to assay:(i) human transforming growth factor-b1 (TGF-b1;DRG International, Inc., USA); and (ii) human inter-leukin-6 (IL-6), human tumor necrosis factor-a (TNF-a), and human interleukin-1b (IL-1b) (all from CLB,Amsterdam, The Netherlands). The sensitivity of theseassays were: TGF-b1, 1.9 pg/ml; IL-6, 0.5 pg/ml; TNF-a,1.0 pg/ml; and IL-1b, 0.8 pg/ml, respectively. Eachexperiment was performed at least four times (N ¼ 8wells/group).
2.11. Evaluation of the rate of extracellular assembly of
collagen fibers in vitro
The rate of extracellular assembly of type I collagenfibers was assessed by assaying by the EIA method ofTaubman et al. [33], as developed by Takara Shuzo Co.,Ltd. (Shiga, Japan), the amount of the C-telopeptidereleased in the process from procollagen type Imolecules. The sensitivity of this assay was 10 ng/ml.Each experiment was performed at least four times(N ¼ 8 wells/group).
2.12. Statistical analysis
A one-way analysis of variance (ANOVA) with posthoc Bonferroni test to compare mean values was appliedto the data and a significance level of 0.05 was chosen.
3. Results
3.1. SF-coated PCU substrates
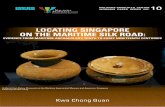
Films were coated by the same lot of regenerated SFsolution (2.8%w/wsolution) obtaining a coating of1.33mg SF/1.0 cm2 of PCU film. The coating appearedto be homogeneous, as can be observed by SEM(Fig. 1A). The presence of SF-coating (thickness200–600 nm) could be detected only in the proximityof a cross section and of coating defects due to samplepreparation (Fig. 1B). At high magnification (2000X)SF surfaces appeared to be slightly rough. However, thereasons for this surface unevenness were not investigatedin the present work and, hence, at present it is notpossible to decide whether it is an artifact or not. Whenincubated in PBS for lengthy terms, the percent fraction(w/coating w) of SF released from the coated PCUsubstrates was low (i.e.o 5%), a finding in keeping withpreviously reported data [18]. This can be ascribed to thecrystallization of the metastable, water-soluble form ofSF induced by MeOH treatment. No changes in SFcoating topography could be observed by SEM afterMeOH exposure.
3.2. Human cell adhesion and growth in vitro
Intravitally labeling with the fluorescent lipophilictracer DiI, which binds to cell membrane phospholipids,permitted the prompt identification of the living cellsthat adhered to either PCU substrate presently investi-gated. Besides, notwithstanding the dwindling of thefluorescence intensity due to the dilution of the cell-bound DiI between the daughter cells at each mitosis,the tracer allowed for a quick reckoning of the actualsize of the cell populations in the cultures (Figs. 1Cand D).The percent cell fraction that within the first 3 h of
incubation adhered to SF-coated PCU specimens was5373 with respect to 2472 for uncoated PCU films(Fig. 2A), indicating that SF-coating significantly(po0:001; n ¼ 4) enhanced the initial cellular bondingto PCU substrates. Subsequently, by day 30 of incuba-tion in vitro absolute cell numbers were 2.5-fold higheron the SF-coated than on the uncoated PCU films(Fig. 2B). By taking as equal to one the correspondingcell numbers at day 4, it became clear that between the4th and the 30th day, the cell population size enlargedby about 13.3-fold on the uncoated PCU films, whileincreasing by 16.5-fold on the SF-coated PCU films (atday 30, +24%, p not significant vs. parallel uncoatedPCU samples). Hence, it was the higher degree of initialcell attachment to substrate due to the SF coating thatwas at the root of the much significantly greater absolutenumbers of human cells found on PCU+SF films.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799792
3.3. Cytokine secretion in vitro
During the first 30 days of incubation in vitro, humanadult fibroblasts sticking to either uncoated or SF-coated PCU films did not secrete any amount detectableby ELISA assays of three main inflammatory cytokines,i.e. IL-1b, TNF-a, and TGF-b1, into the growthmedium (not shown).Conversely, ELISA-assayable amounts of IL-6 were
released into the growth medium by fibroblasts grownon either kind of PCU substrate. Human fibroblastsgrown on SF-coated PCU films secreted far largeramounts of IL-6 than they did when cultured onuncoated PCU surfaces —an event that was statisticallysignificant (po0:01 at least) from the 14th day ofincubation in vitro onwards (Fig. 2C).
3.4. Uptake of d-glucose and l-glutamine and release of
lactate in vitro
The rates of d-glucose consumption were found to bemuch higher in human fibroblasts adhering to SF-coated PCU membranes than in cells on uncoated PCUfilms, with patterns roughly paralleling the respective
rates of cell growth. Again, statistically significantdifferences (p o0.01 at least) were detectable from the14th day of incubation in vitro onwards (Fig. 3A).Conversely, l-glutamine, another important source of
chemical energy for the fibroblasts besides d-glucose[34], was utilized at rather similar rates (p > 0:05 in allpair-wise comparisons) by cells kept on either kind ofPCU substrate (Fig. 3B).It is well established that fibroblasts metabolize
both d-glucose and l-glutamine to lactate [35],which is then discharged into the growth medium.Hence, this metabolic facet too had to be investigated.As shown in Fig. 3C, fibroblasts stuck to SF-coatedPCU films discharged much greater amounts of lactatethan did cells grown on uncoated PCU surfaces, andstatistically significant differences (po0:05 at least) weredetectable from the 8th day of incubation onwards(Fig. 3C).Thus, the enhanced rates of d-glucose consumption
and lactate release as well as the intensified rates of IL-6secretion mirrored the significantly stronger growthactivities characteristic of the human fibroblasts at-tached to SF-coated PCU films as contrasted touncoated ones.
Fig. 1. (A) SEM image (2000� ) of methanol treated SF-coated PCU substrate: a homogeneous surface is visible, even at higher magnifications. (B)
The presence and the thickness of the coating are evident at a coating defect on the upper edge of the substrate (SEM image at 100� ). (C) DiI-
prelabeled fibroblasts cultured on an uncoated membrane (PCU) on their 23rd day of incubation in vitro. 100� . (D) greater numbers of DiI-
prelabeled fibroblasts have grown on an SF-coated PCU (PCU+SF) membrane after 23 days of incubation. In A and B the rims of the substrates are
indicated by arrows, and some cells appear to be out of focus because the surfaces are not perfectly flat.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799 793
3.5. Time-related metabolic changes on a per 105 cells
basis according to the substrate
Since SF-coating promoted much higher degrees ofcell crowding, we deemed to be of interest comparing ona per 105 cells basis the metabolic features of fibroblastsgrown on SF-coated or uncoated surfaces. Thus,between the 4th and 16th day in vitro the utilizationof d-glucose was significantly higher, though progres-sively declining (from 3.44- to 1.5-fold), on the SF-coated PCU films than on the uncoated ones, on whichinstead it remained steady (Fig. 4A). Conversely, duringthe same time lag consumption of l-glutamine washigher (+38–54.2%, po0:01) on the uncoated filmsthan on the SF-coated ones, on which it increased
(+33.3–35%, po0:05) between days 18 and 30, therebybecoming not significantly lower than that on theoncoated substrates (Fig. 4B). Conversely, on the SF-coated PCU films the initially quite low secretion rate ofIL-6 increased linearly by 18.3-fold between the 4th and30th day in vitro, while on the uncoated substrates IL-6release rates were steady for the first 16 days to slowlysurge thereafter (day 30, by 1.4-fold) (Fig. 4C). Finally,while on the uncoated films the rate of extracellularassembly of collagen type I fibers per 105 fibroblasts wassteady between the 4th and 30th day in vitro, on the SF-coated substrates it was significantly higher (from 2.3- to1.7-fold) between days 4 and 14, thereafter declining tomarginally higher levels (from 1.4- to 1.3-fold) betweendays 18 and 30 (Fig. 4D). Therefore, SF-coated PCU
0
15
30
45
60
*
% C
EL
L A
DH
ESI
ON
PCU+SF PCU
0 5 10 15 20 25 300
10
20
30
40
50
60
70
PCU+SF PCU
IL-6
PR
OD
UC
TIO
N (
AR
BIT
RA
RY
UN
ITS)
0 5 10 15 20 25 300
2
4
6
8
10
12
14
16
18
DAYS IN VITRO
DAYS IN VITRO
CE
LL
NU
MB
ER
S (x
105 )
PCU+SF PCU
*
(A) (B)
(C)
Fig. 2. The attachment to uncoated (PCU) or SF-coated (PCU+SF) substrates, the absolute cell numbers, and the IL-6 release of normal human
adult fibroblasts. (A) Percent fractions of fibroblasts adhering PCU or PCU+SF films after a 3-h incubation in vitro; *, po0:001. (B) Growthkinetics of fibroblasts: at all the time points considered, the PCU+SF values differ significantly from corresponding PCU values (po0:05 at least).(C) Cumulative secretion of IL-6 by human fibroblasts; the data have been normalized so that the mean values at day 4 in vitro (i.e., PCU, 68.6 pg/ml;
PCU+SF, 3.1 pg/ml) are taken as equal to one. PCU+SF values differ significantly from corresponding PCU values (po0:05 at least) from the 14th
day of incubation onwards. In A–C, the points on the curves are means7S.E.M. of the values from four distinct experiments.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799794
surfaces appeared to act as an environment that wasmore congenial than the uncoated PCU films to theadhesion, growth, and appropriate operation of thehuman fibroblasts.
4. Discussion
From the present results, it appears that SF-coatingconfers to PCU-based biomaterials indisputable
0 5 10 15 20 25 300
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
PCU+SF PCU
LA
CT
AT
E R
EL
EA
SE (
AR
BIT
RA
RY
UN
ITS)
DAYS IN VITRO
0 5 10 15 20 25 300
1
2
3
4
5
6
7
8
9
10
11
12
13
DAYS IN VITRO
GL
UC
OSE
UPT
AK
E (
AR
BIT
RA
RY
UN
ITS)
PCU+SF PCU
0 5 10 15 20 25 300
1
2
3
4
5
6
7
8
9
10
11
GL
UT
AM
INE
UPT
AK
E (
AR
BIT
RA
RY
UN
ITS)
DAYS IN VITRO
PCU+SF PCU
(A) (B)
(C)
Fig. 3. The time-related changes in the various metabolic activities of human fibroblasts grown on uncoated (PCU) or SF-coated (PCU+SF) films.
(A) Cumulative utilization of d-glucose; the data have been normalized so that the mean values at day 4 in vitro (i.e., PCU, 0.13mg/ml; PCU+SF,
0.29mg/ml) are taken as equal to one. (B) Cumulative uptake of l-glutamine; the mean values at day 4 in vitro (i.e., PCU, 0.23mm; PCU+SF,
0.09mm) are taken as equal to one. At all the time points considered, the PCU+SF values do not significantly (p > 0:05) differ from the
corresponding PCU values. (C) Cumulative release of lactate; the mean values at day 4 in vitro (i.e., PCU, 0.25mg/ml; PCU+SF, 0.74mg/ml) are
taken as equal to one. Points on the curves in A–C are means7S.E.M. of the values from four different experiments.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799 795
advantages from the standpoint of tissue engineering.Hence, SF-coated PCU substrates embody a novel classof biomaterials, the possible manifold biomedicalapplications of which should deserve adequate consid-eration.The effects of PCU+SF substrates on cell culture
were studied with normal human cells; the resultsconfirmed the good cell adhesion and proliferation ofrodent cells [5–7], although they could not be consideredas full substitutes for human cells, and of osteoblast-likeSaos-2 cells [17].Uncoated poly(carbonate)-urethane substrate, e.g.
Bionate, was reported to poorly support cell adhesion[23–25]. However, at partial variance with results fromother laboratories, our data indicate that normal humanadult fibroblasts adhered and proliferated onto Bionateas they would do on tissue culture PST and did not
appear to suffer any damage from cytotoxic actions oragents, as occurred instead for human umbilical veinendothelial cells (HUVEC) [23]. At present, the reasonsfor these discrepancies in behavior between HUVECand normal human adult fibroblasts grown on the samesubstrate, i.e. the uncoated medical grade Bionate 80A,are not understood. The age of the cell donors, anddifferences in the ways the biomaterial samples wereactually handled might have played significant roles,though the relative importance of these and, possibly, ofother yet unidentified factors remain the object ofspeculation and of further research work.Our results show that SF-coated PCU substrates
permitted both a significantly greater adherenceand, consequently, a more intense proliferativeactivity of the human fibroblasts than did uncoatedPCU films. To what extent, if any, these higher
0 5 10 15 20 25 300
5
10
15
GLUCOSE PCUPCU+SF
0 5 10 15 20 25 300
1
2
L-GLUTAMINE PCU PCU+SF
0 5 10 15 20 25 300
100
200
300
400
500 IL-6PCUPCU+SF
DAYS IN VITRO
0 5 10 15 20 25 300
40
80
120
160 PROCOLLAGENC-PEPTIDE
PCUPCU+SF
ng/1
05 ce
llsµm
oles
/105
cells
pg/1
05 ce
llsm
g/10
5 ce
lls
(A) (B)
(C) (D)
Fig. 4. Time-related effects of the type of substrate employed on the metabolic features on a per 105 cells basis. (A) d-glucose uptake. (B) l-glutamine
uptake. In both A and B pair-wise comparisons of PCU vs. PCU+SF values between the 4th and 16th day in vitro, but not those at later time points,
reveal significant differences (po0:05 at least). (C) Secretion of IL-6; excepting for the data on day 14, all the PCU/PCU+SF values are significantly
different (po0:05 at least). (D) Extracellular assembly of type I collagen fibers (assessed by the release of the procollagen C-peptide). Pair-wise
comparisons of PCU vs. PCU+SF values at days 4 and 14, but not at later times, reveal significant differences (po0:02 at least). In A–D points on
the curves are means of the values from four different experiments. S.E.M.’s, not shown, were within 5–12% of the mean values.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799796
degrees of cell crowding on the SF-coated surfaces wereaided by the release into the growth medium of amitogenic cytokine, i.e. IL-6 [36–38], remains to beestablished (see also below).It is well established that normal human adult
fibroblasts utilize both d-glucose and l-glutamine asmajor energy and carbon sources for their survival andgrowth [34,35]. Both fuels are metabolized to lactate ascultured skin fibroblasts are endowed with a highlyglycolytic mode of metabolism [35]. The utilization of d-glucose and of l-glutamine by fibroblasts is reciprocallyregulated [34]. Our findings indicate, as would beexpected, that, with respect to cells kept on uncoatedPCU films, the crowded fibroblasts grown on SF-coatedPCU substrates utilized much larger amounts of d-glucose while releasing greater amounts of lactate. Oncethe effects of cell crowding were excluded, it becameclear that fibroblasts adhering to SF-coated PCUsubstrates initially preferred d-glucose to l-glutamineas their main metabolic fuel, only lately increasing theirconsumption of the latter. Conversely, cells on uncoatedPCU substrates appeared to steadily prefer as a fuel l-glutamine to d-glucose (Fig. 4). However, in eitherinstance, lactate releases depended upon the actualdegree of cell crowding and not on the kind of substrate(not shown). At present, the reasons for these differ-ences in cell metabolism according to the specificsubstrate considered and/or the duration of the stayingin vitro are not understood.Cytokines are signaling molecules of a rather high
number of different species produced and released bycells to control tissue environments and, when needed,to induce local reactive responses. Thus, dermalfibroblasts are known to synthesize and secrete IL-1b,TNF-a, and TGF-b1 [39,40], a set of cytokinesimportantly involved in the modulation of processessuch as skin growth, inflammation, repair, and fibrosisor scarring [41,42]. The ways by which such cytokinesoperate are complex, involving free and cell surface-bound specific receptors and post-receptorial signalingpathways that cross-talk with one another, therebymodifying vital metabolic processes and inducing orsuppressing the production of several other cytokines(see [43] for references). Most importantly, our resultsshow that human fibroblasts adhering to the SF surfacecoat of PCU substrates were not induced under suchcircumstances to secrete measurable amounts of thesethree major proinflammatory cytokines into the growthmedium. The present results are complemented by invitro findings by others suggesting that SF is endowedwith a lesser inflammatory capability than PST andpoly(2-hydroxyethyl methacrylate) do [8]. Clearly, stu-dies on the animals are necessary to reach definitiveconclusions on this topic. Yet, the present resultssupport the hypothesis that SF does not trigger therelease of three main proinflammatory cytokines and,
therefore, once implanted, might be well tolerated byhuman tissues.Conversely, our data show that the contact with SF-
covered surfaces induces normal human adult fibro-blasts to secrete into the medium rather huge amountsof the cytokine IL-6. At this time, the mechanism(s)underlying this enhanced secretion of IL-6 (and possiblyeven of other cytokines) is(are) not understood.Reportedly, IL-6 is a multifunctional cytokine of theIL-6/leukemia inhibitory factor (LIF) family, whoseproduction by fibroblasts occurs under the action ofseveral stimuli, including serum factors [44], platelet-derived growth factor (PDGF) [45], interleukin-1a (IL-1a) [46], IL-1b [47] interleukin-4 (IL-4, which alsoenhances, via the secretion of IL-6, fibroblast prolifera-tion in vitro: [36]), TNF-a [48], TGF-b1 [49], interferon-g (IFN-g) [50], and exposure to UV light [51], todibutyryl 30,50-cyclic adenosine monophosphate(DBcAMP) [52], to metals like copper, zinc, cobalt,nickel, and palladium [53], to hydroxyapatite particles[54], and to cyclic mechanical stretching [36]. By way ofits specific high-affinity functional receptors [47,55], IL-6is known to modulate the proliferation of fibroblasts[36–38], and to enhance the production of collagen,glycosaminoglycans (GAG), interstitial collagenase, andstromelysin-1 by cultured human adult dermal fibro-blasts, thereby favoring wound healing [37,51,56,57] andhypertrophic burn scarring [58]. Moreover, IL-6 par-takes to the mounting and amplification of theinflammatory response in cooperation with otherproinflammatory cytokines, to autoimmune diseases,and to tumor development (see [59] for references). Yet,most interestingly, it should be recalled here that IL-6acts as a potent mitogen for several types of cells,including human keratinocytes, by inducing the expres-sion of keratinocyte growth factor (KGF) in dermalfibroblasts [60]. Hence, since our results show thathuman dermal fibroblasts adhering to SF-coated sub-strates release rather huge amounts of IL-6, one mightsurmise that this cytokine would, in turn, directly orindirectly enhance the proliferation of both fibroblastsand keratinocytes, thereby accelerating the healing ofskin wounds [59].Collagen fibers are assembled extracellularly under
both normal and pathological conditions by cutting theterminal C-peptides of procollagen molecules. Thesynthesis of procollagen molecules is powerfully stimu-lated by TGF-b1, TGF-b2, IL-6 [51,56,57] and serumfactors [40,44], while being repressed by IL-1b andTNF-a; the TGF-b antagonists interferon-a and inter-feron-g; and by dexamethasone [61]. Our finding thatSF-coated PCU substrates did enhance the extracellularassembly of collagen fibers is in keeping with the parallelfinding that fibroblasts grown on SF-coated substrateswere induced to secrete greater amounts of IL-6, whilenot secreting TGF-b1 or IL-1b at all. These data suggest
A. Chiarini et al. / Biomaterials 24 (2003) 789–799 797
that SF would enhance collagen fiber assembly not byitself but indirectly via an increased secretion of IL-6[51,56,57]. This operative mechanism requires furtherstudies to be validated.In conclusion, our present findings show that SF-
coating significantly ameliorates the dealings of normalhuman adult fibroblasts with PCU substrates. There-fore, it appears reasonable to surmise that SF-coatedbidimensional (and tridimensional: manuscript in pre-paration) biomaterials are more advantageous, from thestandpoint of human tissue bioengineering, than theiruncoated counterparts are. Further research, currentlyunder course in our laboratories, will reveal whether thefavorable features exhibited by such composite bioma-terials in vitro hold their promise also in vivo.
Acknowledgements
This work was funded by the Italian Ministry forUniversity and Scientific and Technologic Research(MIUR, Rome; funds allotted: PRIN 1999).
References
[1] Minoura N, Tsukada M, Nagura M. Physico-chemical properties
of silk fibroin membrane as a biomaterial. Biomaterials
1990;11:430–4.
[2] Soong HK, Kenyon KR. Adverse reactions to virgin silk sutures
in cataract surgery. Ophthalmology 1984;91:479–83.
[3] Sakabe H, Ito H, Miyamoto T, Noishiki Y, Ha WS. In vivo blood
compatibility of regenerated silk fibroin. Sen-i Gakkaishi 1989;
45:487–90.
[4] Minoura N, Aiba S, Gotoh Y, Tsukada M, Imai Y. Attachment
and growth of cultured fibroblast cells on silk protein matrices.
J Biomed Mater Res 1995;29:1215–21.
[5] Gotoh Y, Tsukada M, Minoura N. Effect of the chemical
modification of the arginyl residue in Bombyx mori silk fibroin on
the attachment and growth of fibroblast cells. J Biomed Mater
Res 1998;39:351–7.
[6] Inouye K, Kurokawa M, Nishikawa S, Tsukada M. Use of
Bombyx mori silk fibroin as a substratum for cultivation of animal
cells. J Biochem Biophys Methods 1998;37:159–64.
[7] Norihiko M, Sei-ichi A, Yohko G, Masuhiro T, Yohji I.
Attachment and growth of cultured fibroblast cells on silk fibroin
matrices. J Biomed Mater Res 1995;29:1215–21.
[8] Santin M, Motta A, Freddi G, Cannas M. In vitro evaluation of
the inflammatory potential of the silk fibroin. J Biomed Mater
Res 1999;46:382–9.
[9] Kesenci K, Motta A, Fambri L, Migliaresi C. Poly(e-caprolac-tone-co-d,l-lactide)/silk fibroin composite materials: preparation
and characterization. J Biomater Sci Polym Ed 2001;12:337–51.
[10] Liang CX, Hirabayashi K. Improvements of the physical
properties of fibroin membranes with sodium alginate. J Appl
Polym Sci 1992;45:1937–43.
[11] Li M, Lu S, Wu Z, Tan K, Minoura N, Kuga S. Structure and
properties of silk fibroin–poly(vinyl alcohol) gel. Int J Biol
Macromol 2002;30:89–94.
[12] Chen X, Li W, Zhong W, Lu Y, Yu TY. pH sensitivity and ion
sensitivity of hydrogels based on complex-forming chitosan/silk
fibroin interpenetrating polymer network. J Appl Polym Sci
1997;65:2257–62.
[13] Sun Y, Shao Z, Ma M, Hu P, Liu Y, Yu T. Acrylic polymer-silk
fibroin blend fibers. J Appl Polym Sci 1997;65:959–66.
[14] Cai K, Yao K, Lin S, Yang Z, Li X, Xie H, Qing T,
Gao L. Poly(d,l-lactic acid) surfaces modified by silk fibroin:
effects on the culture of osteoblasts in vitro. Biomaterials 2002;
23:1153–60.
[15] Cai K, Yao K, Cui Y, Yang Z, Li X, Xie H, Qing T, Gao L.
Influence of different surface modification treatments on
poly(d,l-lactic acid) with silk fibroin and their effects on the
culture of osteoblast in vitro. Biomaterials 2002;23:1603–11.
[16] Gotoh Y, Tsukada M, Minoura N, Imai Y. Synthesis of
poly(ethylene glycol)–silk fibroin conjugates and surface interac-
tion between L-929 cells and the conjugates. Biomaterials 1997;
18:267–71.
[17] Sofia S, McCarthy MB, Gronowicz G, Kaplan DL. Functiona-
lized silk-based biomaterials for bone formation. J Biomed Mater
Res 2000;54:139–48.
[18] Petrini P, Parolari C, Tanzi MC. Silk fibroin–polyurethane
scaffolds for tissue engineering. J Mater Sci: Mater Med 2001;
12:849–53.
[19] Edwards A, Carson RJ, Szycher M, Bowald S. In vitro and in
vivo biodurability of a compliant microporous vascular graft. J
Biomater Appl 1998;13:23–45.
[20] Tanzi MC, Fare S, Petrini P. In vitro stability of polyether and
polycarbonate urethanes. J Biomater Appl 2000;14:325–48.
[21] Hergenrother RW, Wabers HD, Cooper SL. Effect of hard
segment chemistry and strain on the stability of polyurethanes: in
vivo biostability. Biomaterials 1992;13:240–8.
[22] Zhang Z, King MW, Guidoin R, Therrien M, Doillon C, Dihel-
Jones WL, Huebner E. In vitro exposure of a novel polyether-
urethane graft to enzymes: a study of the biostability of the
vascugraft arterial prosthesis. Biomaterials 1994;15:1129–44.
[23] Zhang Z, Roy R, Dugre FJ, Tessier D, Dao L. In vitro
biocompatibility study of electrically conductive polypyrrole-
coated polyester fabrics. J Biomed Mater Res 2001;57:63–71.
[24] Mathur AB, Collier TO, Kao WJ, Wiggins M, Schubert MA,
Hiltner A, Anderson JM. In vivo biocompatibility and biost-
ability of modified polyurethanes. J Biomed Mater Res 1997;
36:246–57.
[25] Salacinski HJ, Tai NR, Punshon G, Giudiceandrea A, Hamilton
G, Seifalian AM. Optimal endothelialisation of a new compliant
poly(carbonate-urea)urethane vascular graft with effect of phy-
siological shear stress. Eur J Vasc Endovasc Surg 2000;20:342–52.
[26] Belanger MC, Marois Y, Roy R, Mehri Y, Wagner E, Zhang Z,
King MW, Yang M, Hahn C, Guidoin R. Selection of a
polyurethane membrane for the manufacture of ventricles for a
totally implantable artificial heart: blood compatibility and
biocompatibility studies. Artif Organs 2000;24:879–88.
[27] Lin HB, Sun W, Mosher DF, Garcia-Echeverria C, Schaufelber-
ger K, Lelkes PI, Cooper SL. Synthesis, surface, and cell-adhesion
properties of polyurethanes containing covalently grafted RGD-
peptides. J Biomed Mater Res 1994;28:329–42.
[28] Phaneuf MD, Quist WC, LoGerfo FW, Szycher M, Dempsey DJ,
Bide MJ. Chemical and physical characterization of a novel
poly(carbonate urea) urethane surface with protein crosslinker
sites. J Biomater Appl 1997;12:100–20.
[29] Motta A, Armato U, Capuana P, Fambri L, Migliaresi C. Silk
derived fibroin membranes for biomedical use. I. Preparation and
physico-mechanical properties. Third International Symposium
on Frontiers in Biomedical Polymers (FBPS) Including Polymer
Therapeutics—From Laboratory to Clinical Practice—, Shiga,
Japan. Abstracts Book 1999. p. 26.
[30] Armato U, Romano F, Andreis PG, Paccagnella L, Marchesini C.
Growth stimulation and apoptosis induced in cultures of neonatal
rat liver cells by repeated exposures to epidermal growth factor/
A. Chiarini et al. / Biomaterials 24 (2003) 789–799798
urogastrone with or without associated pancreatic hormones. Cell
Tissue Res 1986;245:471–80.
[31] Trinder P. Determination of blood glucose using an oxidase–
peroxidase system with a non-carcinogenic chromogen. J Clin
Pathol 1969;22:158–61.
[32] Barham D, Trinder P. An improved colour reagent for the
determination of blood glucose by the oxidase system. Analyst
1972;97:142–5.
[33] Taubman MB, Goldberg B, Sherr C. Radioimmunoassay for
human procollagen. Science 1974;86:1115–7.
[34] Zielke HR, Ozand PT, Tildon JT, Sevdalian DA, Cornblath M.
Reciprocal regulation of glucose and glutamine utilization
by cultured human diploid fibroblasts. J Cell Physiol 1978;
95:41–8.
[35] Zielke HR, Sumbilla CM, Sevdalian DA, Hawkins RL, Ozand
PT. Lactate: a major product of glutamine metabolism by human
diploid fibroblasts. J Cell Physiol 1980;104:433–81.
[36] Skutek M, van Griensven M, Zeichen J, Brauer N, Bosch U.
Cyclic mechanical stretching enhances secretion of interleukin-6 in
human tendon fibroblasts. Knee Surg Sports Traumatol Arthrosc
2001;9:322–6.
[37] Mateo RB, Reichner JS, Albina JE. Interleukin-6 activity in
wounds. Am J Physiol 1994;266:R1840–4.
[38] Fehgali CA, Bost KL, Boulware DW, Levy LS. Human
recombinant interleukin-4 induces proliferation and interleukin-
6 production by cultured human skin fibroblasts. Clin Immunol
Immunopathol 1992;63:182–7.
[39] Elias JA, Freundlich B, Adams S, Rosenbloom J. Regulation of
human lung fibroblast collagen production by recombinant
interleukin-1, tumor necrosis factor, and interferon-gamma.
Ann N Y Acad Sci 1990;580:233–44.
[40] Varga J, Rosenbloom J, Jimenez SA. Transforming growth factor
beta (TGF beta) causes a persistent increase in steady-state
amounts of type I and type III collagen and fibronectin mRNAs
in normal human dermal fibroblasts. Biochem J 1987;247:
597–604.
[41] Unemori EN, Ehsani N, Wang M, Lee S, McGuire J, Amento EP.
Interleukin-1 and transforming growth factor-alpha: synergistic
stimulation of metalloproteinases, PGE2, and proliferation of
human fibroblasts. Exp Cell Res 1994;210:166–71.
[42] Lee TY, Chin GS, Kim WJ, Chau D, Gittes GK, Longaker MT.
Expression of transforming growth factor beta 1, 2, and 3 proteins
in keloids. Ann Plast Surg 1999;43:179–84.
[43] Revillard J-P, Bona CA, editors. Cytokines and cytokine
receptors. New York: Harwood Academic Publishers, 2001.
[44] Rampino T, Libetta C, Palumbo G, Memoli B, Dal Canton A.
Interleukin-6 production induced in peripheral blood mono-
nuclear cells by a serum factor from IgA nephropathy patients is
inhibited in vitro by specific sugars. Nephrol Dial Transplant
1994;9(11):1560–3.
[45] Takemura H, Suzuki H, Fujisawa H, Yuhara T, Akama T,
Yamane K, Kashiwagi H. Enhanced interleukin-6 production by
cultured fibroblasts from patients with systemic sclerosis in
response to platelet-derived growth factor. J Rheumatol
1998;25:1534–9.
[46] Boxman IL, Ruwhof C, Boerman OC, Lowick CW, Ponec M.
Role of fibroblasts in the regulation of proinflammatory inter-
leukin IL-1, IL-6, and IL-8 levels induced by keratinocyte-derived
IL-1. Arch Dermatol Res 1996;288:391–8.
[47] Waelti ER, Inaebit SP, Rast HP, Hunziker T, Limat A, Braathen
LR, Wiesmann U. Co-culture of human keratinocytes on post-
mitotic human dermal fibroblast feeder cells: production of large
amounts of interleukin-6. J Invest Dermatol 1992;98:805–8.
[48] Butler DM, Feldmann M, Di Padova F, Brennan FM. p55 and
p75 tumor necrosis factor receptors are expressed and mediate
common functions in synovial fibroblasts and other fibroblasts.
Eur Cytokine Network 1994;5:441–8.
[49] Eickelberger O, Pansky A, Mussmann R, Bihl M, Tamm M,
Hildebrand P, Perruchoud AP, Roth M. Transforming growth
factor-beta-1 induces interleukin-6 expression via activating
protein-1 consisting of JunD homodimers in primary human lung
fibroblasts. J Biol Chem 1999;274:12933–8.
[50] Maruyama K, Zhang JZ, Nihei Y, Ono I, Kanako F. Regulatory
effects of gamma-interferon on IL-6 and IL-8 secretion by
cultured human keratinocytes and dermal fibroblasts. J Dermatol
1995;22:901–6.
[51] Brenneisen P, Wlaschek M, Wenk J, Blaudschun R, Hinrichs R,
Dissemond J, Krieg T, Scharffetter-Kochanek K. Ultraviolet-B
induction of interstitial collagenase and stromelysin-1 occurs in
human dermal fibroblasts via an autocrine interleukin-6-depen-
dent loop. FEBS Lett 1999;449:36–40.
[52] Zhou LJ, Ono I. Stimulatory effects of dibyutyryl cyclic adenosine
monophosphate on cytokine production by keratinocytes and
fibroblasts. Br J Dermatol 2000;143:506–12.
[53] Schmalz G, Schuster U, Schweickl H. Influence of metals on IL-6
release in vitro. Biomaterials 1998;19:1689–94.
[54] Ninomiya JT, Struve JA, Stelloh CT, Toth JM, Crosby KE.
Effects of hydroxyapatite particulate debris on the production of
cytokines and proteases in human fibroblasts. J Orthop Res
2001;19:621–8.
[55] Hibi M, Murakami M, Saito M, Hirano T, Taga T, Kishimoto T.
Molecular cloning and expression of an IL-6 signal transducer.
Cell 1990;63:1149–57.
[56] Duncan MR, Berman B. Stimulation of collagen and glycosami-
noglycan production in cultured human adult dermal fibroblasts
by recombinant human interleukin-6. J Invest Dermatol
1991;97:686–92.
[57] Liechty KW, Adzick NS, Crombleholme TM. Diminished
interleukin-6 (IL-6) production during scarless human fetal
wound repair. Cytokine 2000;12:671–6.
[58] Xue H, McCauley RL, Zhang W, Martini DK. Altered
interleukin-6 expression in fibroblasts from hypertrophic burn
scars. J Burn Care Rehabil 2000;21:142–6.
[59] Paquet P, Pierard GE. Interleukin-6 and the skin. Int Arch
Allergy Immunol 1996;109:308–17.
[60] Brauchle M, Angermeyer K, Hubner G, Werner S. Large
induction of keratinocyte growth factor expression by serum
growth factors and pro-inflammatory cytokines in cultured
fibroblasts. Oncogene 1994;9:3199–204.
[61] Mauviel A, Heino J, Kahari VM, Hartmann DJ, Loyau G, Pujol
JP, Vuorio E. Comparative effects of interleukin-1 and tumor
necrosis factor-alpha on collagen production and corresponding
procollagen mRNA levels in human dermal fibroblasts. J Invest
Dermatol 1991;96:243–9.
A. Chiarini et al. / Biomaterials 24 (2003) 789–799 799