M.D. (Anaesthesiology)
-
Upload
khangminh22 -
Category
Documents
-
view
1 -
download
0
Transcript of M.D. (Anaesthesiology)
i
“PROPHYLACTIC PHENYLEPHRINE INFUSION FOR
PREVENTING HYPOTENSION DURING SPINAL ANAESTHESIA
FOR CESAREAN SECTION”
By
Dr. RESHMA K
Dissertation Submitted to the Rajiv Gandhi University of Health Sciences, Karnataka, Bangalore,
in partial fulfillment of the requirements for the degree of
M.D. (Anaesthesiology) Under the guidance of
Dr. KESHAVA RAO. M.D.
Department of Anaesthesiology
A. J. Institute of Medical Sciences
Mangalore
2012
ii
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
DECLARATION BY THE CANDIDATE
I hereby declare that this dissertation entitled “PROPHYLACTIC
PHENYLEPHRINE INFUSION FOR PREVENTING HYPOTENSION DURING
SPINAL ANAESTHESIA FOR CESAREAN SECTION” is a bonafide and genuine
research work carried out by me under the guidance of Dr. KESHAVA RAO. M.D.,
Associate Professor, Department of Anaesthesiology, A.J. Institute of Medical Sciences.
iii
CERTIFICATE BY THE GUIDE
This is to certify that the dissertation entitled “PROPHYLACTIC PHENYLEPHRINE
INFUSION FOR PREVENTING HYPOTENSION DURING SPINAL
ANAESTHESIA FOR CESAREAN SECTION” is a bonafide research work done by
Dr .RESHMA K in partial fulfillment of the requirement for the degree of Doctor of
Medicine in Anaesthesiology.
iv
ENDORSEMENT BY THE HOD AND DEAN OF THE INSTITUTE
This is to certify that the dissertation entitled “PROPHYLACTIC PHENYLEPHRINE
INFUSION FOR PREVENTING HYPOTENSION DURING SPINAL
ANAESTHESIA FOR CESAREAN SECTION” is a bonafide research work done by
Dr RESHMA K under the guidance of Dr KESHAVA RAO M.D., Associate Professor,
Department of Anaesthesiology, A.J. Institute of Medical Sciences.
v
COPYRIGHT
DECLARATION BY THE CANDIDATE
I hereby declare that the Rajiv Gandhi University of Health Sciences, Karnataka
shall have the rights to preserve, use and disseminate this dissertation/thesis in print or
electronic format for academic / research purpose.
© Rajiv Gandhi University of Health Sciences, Karnataka
vi
ACKNOWLEDGEMENT
First and foremost I would to thank GOD for making this possible. It gives me
great pleasure in preparing this dissertation and I take this opportunity to thank everyone
who has made this possible.
I would like to express my deepest gratitude to my PARENTS who prepared me
for life, whose love and blessings made me the person I am today.
It is my distinct honor and privilege to have worked under the able guidance,
continuous supervision and constant encouragement of Dr. KESHAVA RAO M.D.,
Associate Professor, Department of Anaesthesiology, has made this study possible.
It gives me immense pleasure to extend my sincere thanks to my beloved Teacher
and Mentor Dr. KARUNAKARA ADAPPA M.D., DA, Professor and HOD, department of
Anaesthesiology, for his invaluable guidance, advice, and his constant support and
encouragement during the entire course of this study.
I am deeply indebted to Dr. ANITHA.G.BHAT M.D., Associate Professor for her
constant guidance and encouragement throughout the study.
Words fail to express my heartfelt gratitude to the Faculty of Anesthesiology for
their support and encouragement during my study period.
I am extremely thankful to Dr. LATHA SHARMA M.D., Professor and Head,
Department of Obstetrics and Gynaecology, for providing me the cases and support
during my study period.
vii
I sincerely thank the Faculty of Obstetrics and Gynaecology for their constant
guidance and encouragement.
My gratitude and thanks to Dr. RAMESH PAI, MD. The Dean, A.J.Institute of
Medical Sciences, Mangalore, for letting me use the college and hospital facilities and
resources.
I also thank Dr. SALEEM Medical Superintendent for the help and guidance
during the study.
I am extremely thankful to Mr. KOTIAN for assisting me in the statistical
analysis of the study.
I also thank MICROBITS PRINTERS Kankanady, Mangalore for their
technical assistance in making this dissertation presentable.
I thank all my colleagues and friends for their excellent cooperation during the
course of the study.
viii
LIST OF ABBREVIATIONS USED
ASA → American Society of Anaesthesiologist
BP → Blood Pressure
Bdbp → Baseline diastolic blood pressure
bhr → Basal heart rate
Bmbp → Basaline mean blood pressure
Bpm → Beats per minute
Bsbp → Baseline systolic blood pressure
CI → Confidence interval
Cm → Centimeters
CNS → Central Nervous System
CO → Cardiac Output
CSF → Cerebrospinal Fluid
CVS → Cardiovascular System
DAP → Diastolic Arterial Pressure
DBP → Diastolic Blood Pressure
Eq → Equivalent
Etc → Et cetera
H2O → Water
HR → Heart Rate
Hrs → Hours
Ht → Height
IU → International units
Kg → Kilogram
L → litre
ix
LSCS → Lower segment caesarean section
Lts → Litres
MAP → Mean Arterial Pressure
MBP → Mean blood pressure
µg → microgram
mg → milligram
Min → minute
mmHg → millimeter of Mercury
ml → milliliter
mmol → milli mole
NaCl → Sodium chloride
PREOP → Preoperative
Po2 → Partial pressure of Oxygen
S → Seconds
SAB → Subarachnoid Block
SAP → Systolic Arterial Pressure
SBP → Systolic Blood Pressure
SD → Standard Deviation
Sec → Seconds
UA → Uterine artery
UBF → Uterine Blood Flow
Yrs → Years
Vs → Versus
Wt → Weight
W/V → Weight/ Volume
x
ABSTRACT BACKGROUND: Hypotension after spinal anaesthesia for Caesarean section still
remains a common complication. Various methods have been recommended for
prevention and treatment of this problem. However, despite crystalloid or colloid
preloading, hypotension remains a common problem.
Vasopressors are required to treat the spinal induced hypotension among most of
these patients. Studies involving bolus phenylephrine are in plenty but studies pertaining
to prophylactic phenylephrine infusion are sparse.
OBJECTIVES: This study was conducted to evaluate the safety and efficacy of
prophylactic phenylephrine infusion in preventing spinal anaesthesia induced
hypotension.
METHOD: This is a prospective randomized comparative study conducted at the
Department of Anaesthesia, A.J.Institute of Medical Sciences, Mangalore. 50 patients
aged between 20 to 35 years belonging to ASA grade II, scheduled for elective cesarean
sections were randomly allocated into one of the two groups. Group I (n=25) received
intravenous prophylactic phenylephrine infusion at 100µg/min for 3min after spinal
anaesthesia. Then each min SAP was measured and infusion stopped if SAP> baseline
and continued or restarted, if less than or equal to baseline SAP. Intravenous
phenylephrine bolus 100µg was given when SAP is decreased to <80% of baseline.
Group II (n=25) received only intravenous phenylephrine bolus 100µg when SAP
decreased to <80% of baseline. After 1 minute of SAB; HR, SAP and DBP were recorded
xi
every minute till the extraction of the baby. After the delivery of the baby APGAR score
at 1 minute and 5 minutes were noted. Umbilical artery blood was sent for analysis of the
pH. The total volumes of study solutions given up to the time of delivery of the baby were
recorded.
RESULTS: Phenylephrine infusion decreased the incidence (1[3.75%] of 25 versus 25
[100%] of 25), frequency of hypotension compared with control. Heart rate was
significantly slower in the infusion group compared with the control group. Despite a
large total dose of phenylephrine administered to the infusion group compared with the
control group, umbilical artery blood pH and APGAR scores were similar.
INTERPRETATION AND CONCLUSION: a prophylactic infusion of
phenylephrine100 µg/min in patients receiving spinal anaesthesia for elective cesarean
delivery decreased the incidence and frequency of hypotension without any deleterious
neonatal outcome.
KEYWORDS
Prophylactic Phenylephrine; Subarachnoid Block; Bupivacaine; Hypotension, Cesarean
section.
xii
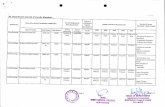
TABLE OF CONTENTS Sl. No.
Page No.
1. INTRODUCTION 1
2 AIMS AND OBJECTIVES 3
3 REVIEW OF LITERATURE 4
4 METHODOLOGY 56
5 RESULTS 62
6 DISCUSSION 82
7 CONCLUSION 89
8 SUMMARY 90
9 BIBLIOGRAPHY 93
10 ANNEXURE
Proforma 99
Consent Form 102
Key to Master Chart 103
Master Chart 104
xiii
LIST OF TABLES
Table No.
Page No.
1. Concentration and doses of bupivacaine 31
2 Comparison of basic parameters between two groups 62
3 Comparison of sensory levels between two groups 65
4 Comparison of HR between two groups of patients 66
5 Comparison of SBP (mmhg) between two groups 68
6 Comparison of DBP (mmhg) between two groups 70
7 Comparison of MBP (mmhg) between two groups 72
8 Comparison of incidence/episodes of hypotension between two groups
74
9 Comparison of dose of phenylephrine between two groups 76
10 Comparison of intravenous fluid administration between two groups 77
11 Comparison of baby extraction time between two groups 78
12 Comparison of baby umbilical artery cord blood pH between two groups
79
13 Comparison of APGAR score between two groups 80
xiv
LIST OF FIGURES
Figure
No. Page No.
1. Features of lumbar vertebra 7
2 Sagittal section through lumbar vertebra 9
3 Spinal Cord 12
4 Arterial supply of spinal cord 14
5 Production, circulation, and resorption of cerebrospinal fluid 16
6 Chemical structure of bupivacaine 28
7 Chemical Structure of phenylephrine 34
xv
LIST OF GRAPHS
Graph No.
Page No.
1. a Age distribution of Patients 62
1.b Height distribution of Patients 63
1.c Weight distribution of patients 63
2 Level of spinal anaesthesia 65
3 Comparison of heart rate among two groups 67
4 Comparison of SBP among two groups 69
5 Comparison of DBP among two groups 71
6 Comparison of MBP among two groups 73
7 Comparison of number of incidence of hypotension among two groups 75
8 Comparison of number of episodes of hypotension among two groups 75
9 Comparison of use of phenylephrine(µg) in two groups 76
10 Comparison of intraoperative fluid use before extraction of the baby between two groups
77
11 Comparison of comparison of duration from skin incision to delivery of baby between two groups
78
12 Comparison of umbilical artery blood pH between two groups 79
13 Comparison of APGAR score at 1 minute between two groups 80
14 Comparison of APGAR score at 5 minute between two groups 81
1
INTRODUCTION
Delivery of a baby by Caesarean section has become increasingly common. A
number of factors account for the increased section rate. It has been commonly accepted
that serious trauma to the baby can be eliminated by avoiding potentially difficult mid-
forceps or vaginal breech delivery and performing a Caesarean section instead. The
widespread use of electronic and biochemical foetal monitoring prior to and during
labour has made it easier to identify a foetus in jeopardy and promptly deliver the baby
by the abdominal route. The clinical impression that Caesarean section is less traumatic
for the tiny foetus and concerns over potential lawsuits in cases of poor neonatal
outcome, have also encouraged obstetricians to perform Caesarean sections with less
positive indication than in the past. Conduction anaesthesia is the most commonly used
anaesthetic for Caesarean section. Spinal anaesthesia appears to be the preferred
technique.1
Although the spinal block offers several advantages like sensory block, muscle
relaxation, minimal risk of aspiration, and a well awake patient to assess clinical
condition, it is often associated with significant adverse effects like hypotension.
Hypotension is one of the commonest problems following spinal anaesthesia for
Caesarean section, potentially endangering both mother and child. Measures to decrease
the incidence and severity of maternal hypotension include left uterine displacement,
fluid preload, prophylactic vasoconstrictors, trendelenburg position and leg compression
etc.2
Traditionally, ephedrine has been the vasopressor of choice in pregnant women.
The use of α-agonists has generally been avoided since the 1970s because of concerns
2
about their potential adverse effect on uterine blood flow. However, in a quantitative,
systematic review of randomized controlled trials of ephedrine versus phenylephrine for
the management of hypotension during spinal anaesthesia for cesarean delivery, Lee and
colleagues showed that there was no difference between ephedrine and phenylephrine in
efficacy. They did find, however, that women given phenylephrine had neonates with
higher umbilical cord blood pH values than women given ephedrine, although the risk of
true fetal acidosis (umbilical pH value of 7.20) was similar in both groups. Because
acidotic changes in the umbilical arterial pH are sensitive indicators of reduced
uteroplacental perfusion, the authors concluded that their finding was indirect evidence
that uterine blood flow may in fact be better with phenylephrine compared with
ephedrine.3
So this randomized study is performed to determine the efficacy of prophylactic
phenylephrine infusion in preventing spinal hypotension following subarachnoid block
for cesarean section in our patient group.
3
AIMS AND OBJECTIVES
1. To determine the efficacy of prophylactic phenylephrine on the incidence of
hypotension in patients receiving spinal anaesthesia for elective cesarean section
2. To determine the effect of the prophylactic phenylephrine on the umbilical artery
blood pH and APGAR score
4
REVIEW OF LITERATURE
HISTORY OF SPINAL ANAESTHESIA 3,4,5,6
The introduction of hollow needle by Rynd F (1844) and a conveniently sized
hollow syringe by Charles Pravaz (18151) paved the way for spinal analgesia.
The concept of local analgesia began with demonstration of anaesthetic properties
of cocaine eye drops by Koller in 1884 and neural blockade by Halsted in 1885.
The term “Spinal anaesthesia” was introduced by Corning in1885. Corning with the
aim of injecting Cocaine between the spinal processes for means of managing neurologic
disorders instead accidentally injected it epidurally in 1885.
The present day spinal anaesthesia and technique of lumbar puncture was described
by Quincke in 1891.
The first two publications on spinal anaesthesia for surgical procedures were made
in 1899 by Bier in the first paper later on by Tuffier. Bier had used it for surgeries on the
lower limbs and Tuffier to relieve pain of sarcoma of the leg in a young man.
Kries in 1900 used spinal analgesia for caesarean section..
In 1905, Pitkin popularized the method of introducing agents intrathecally and in 1927 he
used light and heavy solution and also introduced fine bore, short bevel needle.
Lignocaine synthesized by Lofgren of A B Astra, Sweden in 1943 and used in
clinical practice in 1948.
Bupivacaine was synthesized by A.F.Ekenstein in 1957 used for regional blocks
in 1966.
Chen Schmidt introduced ephedrine in 1923 and used it to maintain blood pressure
(1927) in spinal analgesia.
In 1910 phenylephrine hydrochloride was introduced first by Barger and Dale.
5
APPLIED ANATOMY 3,4,5,6,7
Corning stated in 1900 that “I advise those who contemplate practicing spinal
anaesthesia to take a look at the skeleton especially the relations of the lumbar vertebrae.
An intelligent glance of this sort is worth many words”. The keystone for a successful
spinal anaesthesia lies in the detailed knowledge of the anatomy of the vertebral column
and its contents.
ANATOMY OF SPINE
The vertebral column
Consists of 33 vertebrae
• Cervical - 7
• Thoracic - 12
• Lumbar - 5
• Sacral - 5 (Fused)
• Coccygeal - 4 (Fused)
The curves of the spine
In the adult, the normal spinal column has 4 curves:
1. The cervical curve - convexity anteriorly.
2. The dorsal curve - convexity posteriorly.
3. The lumbar curve - convexity anteriorly.
4. Sacrococcygeal curve - convexity posteriorly.
6
Typical lumbar vertebra consists of
A body - which is weight bearing and separated from adjoining vertebral bodies
by intervertebral disc.
Two pedicles - strong and directed backwards from the upper part of the body.
Two laminae - meeting posteriorly and enclosing the vertebral foramina.
Spinous process: Thick, broad and quadrilateral.
Four articular surfaces, two superior and two inferior, project respectively
upwards and downwards from the junction of the pedicle and lamina.
Two transverse processes homologous with ribs.
8
Contents of Vertebral Column
Roots of spinal nerves
Spinal membranes with their enclosed cord and cerebrospinal fluid.
Structures: Vessels, fat and areolar tissue of the extradural space.
Vertebral ligament bounding the canal
It is essential for the anaesthetist practicing spinal anaesthesia to have an accurate
knowledge of those ligaments in the vertebral column through which spinal needle
passes. The different sensations of resistance that these ligaments impart to the advancing
needle can with practice be appreciated by the operator.
Supraspinous ligament: Is a continuation of Ligamentum Nuchae and joins together
the tips of the spinous processes from the 7th cervical vertebra to the sacrum. It is
thickest and widest in the lumbar region.
Interspinous ligaments: These ligaments connect adjoining spinous processes from
their tips to roots. They fuse with the supraspinous ligaments posteriorly and with
Ligamentum Flavum anteriorly. In the lumbar region they are wide and dense.
Ligamentum Flavum: It is composed of yellow elastic fibres which accounts for its
name. It is placed on either side of spinous process and extends laterally to blend with
capsule of the joints between the superior and inferior articular processes. It runs from
anterior and inferior aspects of lamina above to the posterior and superior aspects of
lamina below. It comprises over half of the posterior wall of the vertebral canal, the
bony laminae accounting for the remainder. Ligamentum Flavum is thinnest at
cervical region and thickest at lumbar region. Functionally these ligaments are muscle
9
spares, assisting in recovery of the effect of posture after bending and in maintaining
erect posture.
Posterior longitudinal ligaments: Lies within the canal on posterior surfaces of
bodies of vertebrae from which it is separated by basivertebral veins. This ligament is
thinnest in cervical and lumbar region.
Anterior longitudinal ligament: It is more of anatomical interest than anesthetic
interest. It runs along the front of vertebral bodies, as also to the intervertebral discs,
to which it is adhered.
Midline spinal puncture pierces the supraspinous, interspinous ligaments and
Ligamentum Flavum. In the lateral approach only Ligamentum Flavum is encountered.
Figure 2: Sagittal section through lumbar vertebra
10
Spinal cord
The elongated part of the central nervous system which occupies upper two thirds
of the vertebral canal and is 42-45 cm long. Extent is from upper border of atlas to the
upper border of the second lumbar vertebra and still lower in infants. At its rostral end,
continues with medulla oblongata, below it ends in conus medullaris from apex of which
filum terminale descends as far as coccyx. The cord has two enlargements- cervical and
lumbar- corresponding to the nerve supply of the upper and lower limbs. The cervical
enlargement extends from C3 to T2 and lumbar enlargement from T9 to T12.
Spinal segments
Spinal cord is divided into segments by a pair of spinal nerves, which arise from
the cord. There are 31 pairs of spinal nerves as follows: eight cervical, twelve thoracic,
five lumbar, five sacral and one coccygeal. The nerve roots within the dura have no
epineural sheath and are therefore easily affected by doses of analgesics drugs brought
into contact with them.
Spinal meninges
Spinal cord is ensheathed by three membranes from without inwards:
• Dura mater
• Arachnoid mater
• Pia mater
Dura mater
A strong fibrous layer forming a tubular sheath attached above to margin of
Foramen Magnum and ending below at the lower border of the second sacral vertebra. It
11
is separated from the bony wall of the vertebral canal by extradural space, which contains
fat, areolar tissue, venous plexus, anterior and posterior roots of spinal nerves. Its main
fibres are longitudinal so that lumbar puncture needle should be introduced with its
needle separating rather than cutting the fibres.
Arachnoid mater
This is a membrane of spider web delicacy which lines dural sheath and which
sends prolongation along each nerve root, subdural space being merely a capillary layer.
Pia mater
This is the inner most of the three membranes, is a vascular connective tissue
sheath, which closely invests the brain, spinal cord and projects into their sulci and
fissures. This is separated from the arachnoid mater by subarachnoid space filled with
CSF. The spinal pia is thickened anteriorly into the Linea Splendens along the length of
anterior median fissure; on either side it forms the Ligamentum Denticulatum, a series of
triangular fibrous strands. The Pia mater ends as a prolongation, Filum Terminale,
which pierces the distal end of the dural sac and is attached to the periosteum of the
coccyx.
13
Blood supply
The arteries supplying the spinal cord are the anterior and posterior spinal arteries,
both of which descend from the level of Foramen Magnum. The anterior spinal artery is a
midline vessel lying on the anterior median fissure in the substance of the pia mater. It is
formed by the union of a branch from each vertebral artery. It is the larger of the two
vessels and supplies the lateral columns, anterior columns and 3/4th of the substance of
the cord. The posterior spinal arteries comprise two vessels on either side derived from
posterior inferior cerebellar arteries. They supply posterior columns on either side. These
arteries are reinforced by arteries, which pass through the intervertebral foramina from
the vertebral, ascending cervical, posterior intercostal, lumbar and lateral sacral arteries.
Spinal veins are gathered together into the anterior and posterior venous plexus. They
drain along the nerve roots, through intervertebral foramina into vertebral, azygous and
lumbar veins.
Nerve supply of the meninges
The posterior aspect of the dura and arachnoid mater contains no nerve fibres and
so no pain is felt on dural puncture. The anterior aspect is supplied by sinovertebral
nerves, each of these enters an intervertebral foramina and passes up for a segment and
down for two segments.
15
THE SUBARACHNOID SPACE 4,7, 8,9
This is the space lying between the arachnoid and pia mater. It consists of the
spinal nerve roots, denticulate ligaments, cerebrospinal fluid, and spongy reticulum of
fibers connecting the pia with the arachnoid mater.
The nerve roots within the dura have no epineural sheaths and are therefore easily
affected by analgesic drugs. The posterior aspect of the arachnoid and dura have no nerve
supply. So there is no pain experienced on dural puncture.
THE CEREBROSPINAL FLUID (CSF)
Cerebrospinal fluid is a modified tissue fluid present in the cerebral ventricles,
spinal cord and subarachnoid spaces. It is produced by choroid plexus in the lateral, third
and fourth ventricles by a combination of filtration and secretion, and later absorbed in
arachnoid granulations over the cerebral hemispheres. In adults the normal total CSF
production is about 21 ml /hr (500 ml /day),about 130 to 150 ml is present at all times of
which 25-35 ml is present in the vertebral canal. The normal CSF pressure measured with
the patient lying in lateral position is 7 –15 cm of water.
17
COMPOSITION OF CSF
Specific gravity: 1.005(1.003- 1.007) at 37degree Centigrade.
pH: 7.33
Volume: 120-140 ml
Glucose (Fasting): 2.5 –4.5 mMOl/L
Sodium: 144-152 miliEq/L
Calcium: 1.1-1.3 miliEq/L
Chloride: 123-128 miliEq/L
Bicarbonate: 24-32 miliEq/L
Proteins: 200-400 mg/l
Urea: 2.0-7.0 miliMOL/L
Osmolality: 289 miliMOL/kg of H2O
FUNCTIONS OF CSF
1. It acts as a buffer separating the brain and the spinal cord from the hard bony skull
and the vertebral canal.
2. Nutrition and oxygen supply to the nerve cells to some extent.
3. Drainage of metabolites.
4. pH changes in CSF, regulates pulmonary ventilation.
5. Reduces effective weight of the brain.
18
APPLIED PHYSIOLOGY
Physiology of Central Neural Blockade
The physiological response to intradural blockade results from autonomic
blockade with its major effects on both the vascular beds and cardiac action; from
abolition of somatic pain and its reflex mediated response, and blockade of motor fibers.
Order of blockade of nerve fibers 6:
First to be blocked is autonomic pre ganglionic nerve fibers (B fibers).
Second to be blocked are temperature and pain fibers (A δ and C fibers).
Third to be blocked pinprick fibers.
Fourth to be blocked fibers conveying pain greater than pinprick.
Fifth to be blocked touch fibers (A β fibers).
Sixth to be blocked deep pressure fibers.
Seventh to be blocked somatic motor fibers.
Eight to be blocked, fibers conveying vibratory sense and proprioception impulses
(A γ fibers).
During recovery, return of sensitivity in the reverse order was assumed, but it has
been suggested that sympathetic activity returns before other sensation . The most
important physiologic response to spinal anaesthesia involves the cardiovascular system;
they include hypotension and bradycardia .
Physiology Of Spinal Hypotention 10, 11, 12,13,14,15
Hypotension is defined as a decrease in SBP >25% from the baseline values or a
SBP <100mm Hg.1
19
Understanding the mechanisms involved in control of arterial pressure in a normal
individual and the pathophysiology of hypotension during spinal anaesthesia is the key to
safe and appropriate management of the patients.
Control of Arterial Pressure12:
Arterial pressure: is the product of cardiac output and systemic vascular resistance and
both these variables are influenced by many other factors.
Cardiac output: is determined by venous return according to Frank Starling law. Venous
return is influenced by gravity, the calf muscle pump, intrathoracic pressure and the
degree of venomotor tone; this is matched to the circulating blood volume.
Systemic Vascular Resistance: is determined by sympathetic vasomotor tone and by the
influence of hormones such as rennin, angiotensin, aldosterone and antidiuretic hormone.
The vasomotor centre in the brain stem controls the degree of sympathetic tone in a
feedback loop involving the baroreceptors.
Organ Perfusion
There are two main mechanisms which control autoregulation and perfusion they are:
Myogenic autoregulation: acts via stretch receptors in the vessel walls which cause
them to constrict when pressure is decreased.
Chemical autoregulation: is mediated by the local concentration of vasoactive
metabolites. In the presence of vasodilatation, as produced by sympathetic block, an
increase in flow washes out the metabolites and produces reflex vasoconstriction.
Although it is arterial pressure that we measure and adjust, it is important to
remember that organ flow is the vital factor. Compensatory mechanisms mentioned
before ensure that the flow to vital organs is maintained over a wide range of pressures.
20
Cerebral blood flow: Autoregulation occurs between 50 to 150mm Hg mean arterial
pressure. Since these vessels are devoid of sympathetic nerve supply they autoregulate by
myogenic mechanism. The stimulation of vasomotor centre leads to increase sympathetic
tone and systemic vascular resistance in an attempt to restore arterial pressure.
Coronary blood flow: It is mainly mediated by chemical autoregulation between 60 to
150 mm Hg mean arterial pressure. As the cardia becomes hypoxic, adenosine
diphosphate gets accumulated. This gets converted to adenosine, a potent coronary
vasodilator, restoring the local blood flow.
Renal autoregulation: occurs between 60 to 160mm of Hg mean arterial pressure. The
afferent glomerular arteriole has a myogenic response to stretch and constricts with
hypertension and dilates with hypotension.
Primary Mechanisms of Hypotension are :2
(a) Sympathetic preganglionic denervation leading to peripheral venous pooling and
decreased venous return.
(b) Vasodilatation of arterioles and post arteriolar capillaries
(c) Catecholamine depletion due to sympathetic denervation to adrenal medulla (T8 to
L1).
(d) Splenic venous pooling.
(e) Compression of great vessels within abdomen due to muscular paralysis, which is
exaggerated by pregnant uterus and abdominal tumors.
(f) High blocks lead to sympathetic nerve block to the cardia (T1-T4) leads to decreased
contractility.
21
Opposing Factors Affecting Heart Rate are 13,14:
The decrease in systolic arterial pressure which causes a baroreceptor reflex and
an increase in heart rate
i. Changes in the preload causing volume receptor reflexes which alter heart rate
ii. Vagal responses which reduce heart rate.
iii. Sympathetic block of Cardio-acceleratory nerves causing a reduction in heart rate.
iv. The central effect of reduced sensory input to the cortex resulting from subarachnoid
block which reduces heart rate.
v. The specific actions on heart rate of the different treatments used in the prevention
and treatment of hypotension.
The major factor in the development of hypotension is the level of blockade of
sympathetic outflow tract, which is between T1 to L2.Sympathetic preganglionic efferent
blockade which extends 2 to 6 dermatomes cephalad to sensory block leads to venous and
arteriolar dilation, among which venodilation predominates; this is because of limited
amount of smooth muscle in venules and large amount of blood in venous capacitance
(approximately 75% of total blood volume).
The body senses this fall by the baroreceptors present in carotid sinus and aortic
arch and tries to compensate by tachycardia (Marey’s law).
If the sympathetic blockade extends above fifth thoracic vertebrae level it
becomes progressively difficult to compensate as the cardio accelerator fibers arising
from T1 to T4 are also blocked. Additionally the heart rate may further decrease as a
result of fall in right atrial filling. Hypotension usually occurs in the first 10-15 minutes
22
following spinal anaesthesia. Fall in blood pressure is more marked in higher levels of
block, geriatric group, pregnancy, hypertensive and hypovolumic states.
Pregnancy induces various changes in anatomy and physiology, which has a
bearing on conduct of regional anaesthesia and drug pharmacokinetics and
pharmacodynamics.
There are several ways in which use of regional anaesthesia differ for parturients
from their use in non-parturients. Additionally, regional anaesthesia in the mother may
affect the Uteroplacental unit and the foetus.
Decreased plasma proteins and altered protein binding in pregnancy may change
free drug to total drug ratios of anaesthetic agents. For example, protein binding of
Lidocaine decreases throughout pregnancy.
Pregnancy-induced neurohumoral changes may alter responses to pain. Pregnancy
is associated with lower plasma substance P concentrations and higher plasma and
cerebrospinal fluid (CSF) Progesterone levels. Both of these compounds have significant
roles in pain modulation. Nerves from pregnant individuals appear more susceptible to
local anaesthetic blockade. Proposed mechanisms include hormone related changes in the
actions of spinal cord neurotransmitters, potentiation of the analgesic effect of
endogenous analgesic systems, increased permeability of the neural sheath, or other
pharmacodynamic or pharmacokinetic differences between pregnant and nonpregnant
women.
The central nervous system and cardiac toxicity of local anaesthetics are not
altered by pregnancy. Pregnancy produces various anatomical changes in the mother,
which may affect regional anaesthesia technique. The epidural and vertebral foraminal
23
veins are enlarged, which along with increased intra abdominal pressure may lead to
decreased lumbosacral CSF volume. This decreased lumbosacral CSF volume is
associated with increased sensory blockade after spinal anaesthesia.
Hormonal changes affect vertebral ligamentous structures and may make the
Ligamentum Flavum feel softer. The pregnant patient may not flex her lumbar spine
optimally, which may narrow the interspinous spaces and move the line between
interiliac crests more cephalad. Pregnancy-induced widening of pelvis may result in a
head down tilt of spine in the lateral position, potentially affecting the spread of
intrathecal drugs. Parturients may have presacral oedema, making landmark identification
more difficult. Finally, lumbar lordosis and thoracic kyphosis are altered during
pregnancy, perhaps changing the distribution of spinal anaesthetics.
Pregnancy produces various changes in the cardiovascular system. It causes 40-
50% increase in plasma volume and 30-50% increase in cardiac output. Blood pressure
may decrease due to decrease in systemic vascular resistance. Aortocaval compression
produced by enlarged uterus becomes progressively more important reaching its
maximum at 36-38 weeks, after which it may decrease as foetal head descends into the
pelvis. Supine hypotension syndrome, which is seen on lying supine due to compression
of lower aorta by enlarged uterus, may be avoided by uterine displacement or lateral
pelvic tilt. Pregnancy alters the haemodynamic response to endogenous and exogenous
sympathomimetics.
24
Uteroplacental blood flow
Uteroplacental blood flow (UBF) is not autoregulated and is largely dependent on
maternal blood pressure. Neuraxial anaesthesia may affect UBF by a number of
mechanisms. Pain causes activation of the sympathetic nervous system. In pregnant
patients, acute stress increased plasma norepinephrine levels by 25% and decreased UBF
by 50% where as labour analgesia is associated with a marked reduction in circulating
catecholamine levels. Pain also causes maternal hyperventilation. Hyperventilation may
decrease UBF.
Neuraxial anaesthesia has been associated with uterine hypertonus, resulting in a
decrease in UBF and foetal bradycardia. Neuraxial anaesthesia-induced sympathetic
blockade does not appear to alter UBF in normal parturients in the absence of
hypotension. In the settings of maternal hypotension, uterine arterial pressure decreased
whereas uterine vascular resistance increased secondary to reflex release of
vasoconstrictors.
25
PREVENTION AND TREATMENT OF SPINAL HYPOTENSION16,17
Several measures have been recommended to prevent and treat hypotension
following conduction anaesthesia in Obstetrics. Following are a few among them:
Prevention of Hypotension
1. Volume preloading: Preloading with crystalloid or colloid solutions as prophylactic
method to prevent hypotension following spinal anaesthesia is effective in bringing
down the incidence of hypotension even though it cannot eliminate it completely.
Intravenous infusion of balanced, non-dextrose containing solution within 30 minutes
of conduction anaesthesia increases the blood volume and improves the circulation. It
is considered that colloid solutions are better choice in preventing hypotension than
the crystalloid group because colloid when given intravenously will stay in the
intravascular compartment for longer time due to their higher molecular weight than
do crystalloids.
2. Vasopressor as prophylactic measure to prevent hypotension following spinal
anaesthesia: Prophylactic vasopressor administration is recommended with spinal
anaesthesia for Caesarean section. Present recommendations support the use of
phenylephrine, a pure α agonist, as the primary vasopressor. ephedrine, which is an α
and β agonist, had been the gold standard for prophylaxis and treatment of spinal
hypotension. Recent evidence shows that doses of ephedrine large enough to maintain
homeostasis after the induction of spinal anaesthesia may be detrimental to the fetus.
Ephedrine also caused significant hypertension and tachycardia in mothers when used
to treat spinal hypotension. Phenylephrine, a pure α agonist is as efficient as
ephedrine in restoring and maintaining maternal BP. Smaller doses are required
compared to ephedrine and it does not cause clinically significant decrease in uterine
26
blood flow. It does not cause maternal tachycardia but does cause bradycardia as a
physiological effect.
3. Left uterine displacement: Continuous left uterine displacement using a wedge (>15)
under the right hip to minimize aortocaval compression, typically restores venous
return from the lower body and corrects hypotension.
4. Frequent Monitoring: The safety of the above measures as prophylaxis for
hypotension is assured with frequent monitoring.
Therapy
Therapy for spinal hypotension includes:
1. More left uterine displacement.
2. Head down position: This is a simple and effective measure. Gravity will increase
the venous refilling of the heart and the pulmonary blood volume. The result is an
increase in stroke volume and cardiac output with a rise in blood pressure. It was
first used extensively and recommended by Koster, and its value has subsequently
been established by Gordh.
3. Intravenous fluids: Administration of fluids intravenously increases the blood
volume and improves the circulation.
4. Administration of oxygen: Administration of oxygen to the mother may not
necessarily raise the foetal PaO2 until the hypotension is corrected.
5. Vasopressor therapy: This is considered the keystone to the therapy of
hypotension when other simple methods mentioned above fail to do so.
Vasopressor action may be manifested by four mechanisms:
Through vasoconstriction by direct action on arteriolar muscle.
Through central vasomotor stimulation.
Through increased cardiac output by myocardial stimulation.
Through constriction of veins and increasing venous return.
27
APGAR SCORE:
APGAR score was developed in 1952 by an anesthesiologist named Virginia
Apgar. The APGAR test is usually given to your baby twice: once at 1 minute after birth,
and again at 5 minutes after birth. Rarely, if there are concerns about the baby's condition
and the first two scores are low, the test may be scored for a third time at 10 minutes after
birth. Five factors are used to evaluate the baby's condition and each factor is scored on a
scale of 0 to 2, with 2 being the best score:
Respiratory rate- None (0), Slow, Irregular (1), Good (3)
Heart rate/min- Absent (0), <100 (1), >100(2)
Color of the body- Blue or Pale (0), Body pink and extremities blue (1), Pink (2)
Muscle tone – Flaccid (0), Some flexion (1), Actively moving the extremities (2)
Reflex stimulation- No Response (0), Grimace (1), Cries or Coughs (2)
The test was designed to quickly evaluate a newborn's physical condition after
delivery and to determine any immediate need for extra medical or emergency care.
28
PHARMACOLOGY
BUPIVACAINE18,19,20,21:
Local anesthetics are drugs that produce reversible depression of nerve
conduction when applied to nerve fiber. 18
Local anesthetics consist of a liphophilic group; usually a benzene ring- separated
from the hydrophilic group usually a tertiary amine by an intermediate chain that includes
an ester or amide linkage
Bupivacaine has probably had the greatest influence on the practice of regional
anaesthesia due to the combined properties of an acceptable onset, long duration of
action, profound conduction blockade, and significant separation of sensory to motor
block.
It was synthesized by Ekenstein in 1957 and used in clinical practice by Widman
and Telino in 1963.
Chemistry:
Bupivacaine is 1-n-butyl-DL-piperidine-2-carboxylicacid-2, 6 dimethylanilide
hydrochloride. Bupivacaine is a homologie of mepivacaine with molecular formulae of
C18 .N2O.H28.Hcl, differing only in a butyl group substituted for a methyl group on the
piperidine nitrogen.
Chemical structure:
Figure.6: Chemical structure of bupivacaine.
29
Physiochemical Properties:
The base is sparingly soluble, but the hydrochloride salt is readily soluble in
water. Bupivacaine is highly stable and can withstand repeated autoclaving.
Mechanism of Action:
The primary action of local anesthetics is on the cell membrane of the axon. The
large transient increase in the permeability to sodium ions, necessary for propagation of
impulses is prevented. Thus the resting membrane potential is maintained and
depolarization in response to stimulation is inhibited.
The mechanism by which local anesthetics block sodium conductance is as
follows:
(a) Local anesthetics in the cationic form act on the receptors within the sodium
channels, on the cell membrane and block it. The local anesthetics can reach the
sodium channels either via the lipophilic pathways directly across the lipid
membrane or via the axoplasmic opening. The mechanism accounts for 90% of
nerve blocking effects of amide local anesthetics.
(b) The second mechanism of action is by membrane expansion. This is a nonspecific
drug receptor interaction
Anaesthetic Properties:
(a) Potency: Bupivacaine is approximately three to four times more potent than
Lidocaine or Mepivacaine and eight times more than Procaine. It appears to have
a slow nerve penetrating power leading to slow onset, more prolonged duration of
sensory anaesthesia due to its lipid solubility and protein binding properties.
Muscle relaxation is not profound with 0.5% as seen with Lidocaine.
30
(b) pKa: is 8.2.
(c) pH of saturated solution is 5.2
(d) Anaesthetic Index: It is defined as ratio between potency/toxicity of a local
anaesthetic drug. It is 3.0 to 4.0 for Bupivacaine.
Pharmacodynamics:
Onset of action is between 3 to 4 minutes and complete spinal anaesthesia ensues
by 6 to 8 minutes. The duration of spinal anaesthesia varies from 75 to 150 minutes.
Pharmacokinetics:
Plasma levels of the drug depend on the route, concentration and the total dose
administered. The amount of drug absorbed is minimal when administered through
subarachnoid route, plasma bupivacaine concentrations within 1 to 2 hours after
administration is 1 to 2µg/ml. Bupivacaine is distributed throughout all body tissues. T½
α of bupivacaine is 2-7 minutes. T ½ β is 28minutes, T ½ γ is 3-5hrs. Volume of
distribution is 72 lts; clearance is 0.47lt/min. The more highly perfused organs show a
higher concentration of the drug. The blood concentration of the drug decreases markedly
as it passes through the pulmonary vasculature.
Plasma Binding: About 90 to 95% of the drug is bound to protein, unbound drug
is about 1/7 that of Lidocaine and 1/5 that of Mepivacaine.
Metabolism and Elimination:
Bupivacaine is an amide; liver is the primary site of metabolism. It is metabolized
by N-dealkylation and the metabolite, pipecolyloxylidine is excreted in the urine. About
10% of the drug is excreted unchanged in the urine and the remaining is conjugated with
glucuronide and excreted
31
Dose:
Suggested maximum safe dose of Bupivacaine in a 70kg adult with adrenaline is
225mg that is 2.5 to 3.0mg/kg and without adrenaline 175mg that is 2 to 2.5mg/kg body
weight.
Table No. 1: Concentration and doses of Bupivacaine 21
Type of Block
Concentration (In percent %)
Dose (in ml)
Dose (in mg)
Local infiltration 0.25-0.5 25-30 2
Minor nerve block 0.25 5-20 12.5-50
Major nerve block 0.25-0.5 30-50 400
Epidural 0.25-0.75 15-30 37.5-225
Spinal
0.5
0.75
3-4
2-3
15-20
15-22.5
Actions on different systems:
a) Central nervous system:
An overdose of bupivacaine produces light-headedness and dizziness followed by
visual and auditory disturbances such as difficult to focus and tinnitus. Disorientation and
drowsiness can also occur. Shivering, tremors of muscles of face and distal part of the
extremities can occur. Ultimately generalized convulsions of tonic-clonic nature can
occur. Further increase in dose causes respiratory arrest.
b) Cardio vascular system:
Electrophysiological studies on the effect of local anesthetic have demonstrated
that bupivacaine is associated with more pronounced depolarization changes.
Bupivacaine blocks cardiac sodium channels and alters mitochondrial function. Its high
32
degree of protein binding makes resuscitation prolonged and difficult. Bupivacaine is
highly arrythmogenic. This drug reduces the cardiac contractility. This is done by
blocking the calcium transport. Low concentration of bupivacaine produces
vasoconstriction while high doses cause vasodilatation.
c) Autonomous nervous system:
Myelinated preganglionic β fibers are more sensitive to the action of local
anesthetic including bupivacaine. Involvement of preganglionic sympathetic fibers is the
cause of widespread vasodilatation and subsequent hypotension that occurs in epidural
and paravertebral block. When used for conduction blockade, all local anesthetics
particularly bupivacaine produce higher incidence of sensory than motor block.
d) Respiratory system:
Respiratory depression may be caused if excessive plasma level is reached which
in turn results in depression of medullary respiratory centers. Respiratory depression may
also be caused by paralysis of respiratory muscles as may occur in high spinal or total
spinal anaesthesia.
e) Neuro-muscular junction:
Local anesthetics can affect transmission at neuro-muscular junction and block
motor nerve fibers if present in sufficient concentration.
Toxicity:
Local anesthetics are relatively safe if administered in appropriate dosage in the
correct anatomical location. However accidental intravascular, intrathecal injection or
administration of excessive doses results in toxicity.
33
In humans bupivacaine is about 4-5 times more toxic than lidocaine and they
manifest by their effects on the CNS and CVS. The CNS effects are characterized by
excitation or depression. The first manifestation may be nervousness, dizziness, blurred
vision or tremors followed by convulsions, unconsciousness and probably respiratory
arrest.
Other effects may be nausea, vomiting, chills, constriction of the pupils and
tinnitus. The CVS manifestations include myocardial depression, hypotension and
cardiac arrest. In obstetrics, fetal bradycardia may occur. Allergic reactions include
urticaria, bronchospasm and hypotension.
Treatment of toxic reactions:
Treatment is mainly symptomatic. Main goal of treatment is to maintain near
normal circulation and to support ventilation with oxygen or controlled ventilation if
required. Supportive treatment with intravenous fluids and vasopressors restore the
cardiovascular stability, convulsions may be controlled with diazepam or thiopentone
sodium and controlled ventilation with oxygen. A rapid bolus of Intralipid 20%,
1.5 mL/kg (or roughly 100 mL in adults), be administered without delay, followed if
necessary by an infusion of 0.25 mL/kg/min for the next 10 minutes. Corticosteroids may
be helpful when allergic reactions are suspected
34
PHENYLEPHRINE:22,23,24,25
Phenylephrine is a relatively selective α-1 adrenoreceptor agonist.
Chemistry: Phenylephrine hydrochloride – C9.H13.NO2.Hcl
1. - 3 – hydroxy- α- [(methylamino)methy] benzenemethanol
Chemical structure:
Figure 7: Chemical structure of phenylephrine
Molecular weight 203.7(167.2)
pKa (-OH,-NH-) 8.9,10.1
Solubility In water
In alcohol
1 in 2
1 in 4
Octanol/water partition coefficient -
Phenylephrine hydrochloride is an odorless, bitter tasting, white crystalline
powder which is prepared by chemical synthesis. It is available for use by oral , topical
and parenteral administration.
35
Pharmacology:
Phenylephrine is considered a relatively selective α1 adrenoreceptor agonist. It is
known to have some weak α2 adrenoreceptor agonist activity and some activity as a β
adrenoreceptor agonist. Most of α stimulant activity is the result of a direct action on the
receptor and relatively little caused by the indirect effect via release of norepinephrine.
The α1 adrenoreceptor action is slightly stronger than the venous capacitance vessels
when compared to the arteriolar resistance vessels.
Toxicology:
There is no evidence to indicate mutagenic potential and teratogenicity testing in
the dog has suggested that it is not likely that any sizable amount crosses the placenta.
There is no reported carcinogenicity.
Clinical Pharmacology
Phenylephrine is a preferred α1 adrenoreceptor agonist drug, leading to dose and
concentration dependent vasoconstriction.
It causes increase in the blood pressure with a reflex bradycardia. Cardiac output
doesnot normally fall, but may if there is ischemic heart disease. There is no significant
CNS effect and there is no significant increase in energy expenditure. The reflex
bradycardia can be antagonized by atropine. There is a reduction in blood flow to the
renal, cutaneous, splanchnic, and skeletal muscle vascular beds. Coronary artery
vasoconstriction occurs, but overall blood flow is usually little affected and may actually
increase, especially if perfusion pressure is initially low.
The pressor effect can be antagonized by selective α1 antagonist. Conversely, the
effect of clonidine, an α2 agonist, is to potentiate the pressor response of intravenous
36
phenylephrine, by increasing the post junctional α1 adrenoreceptor mediated
vasoconstriction.
Pharmacokinetics:
Phenylephrine is variably absorbed after oral administration and is also subject to
extensive presystemic metabolism as a consequence, systemic bioavailability is only
about 40%, with peak plasma concentrations at 1-2hr.
Oral absorption Irregular
Presystemic metabolism 60%
Systemic bioavailabitlty 40%
Plasma half life 2-3hr
Volume of distribution 200-500l
Plasma protein binding unknown
Metabolism:
Phenylephrine undergoes extensive biotransformation in the intestinal wall during
absorption. Following absorption; the drug is extensively biotransformed in liver. Both
phenylephrine and its metabolites are excreted in urine, with only small amount of drug
excreted unchanged. The metabolites of phenylephrine are not active.
The principal routes of metabolism are to sulfate conjugates, which are formed
largely in gut wall, and oxidative deamination by monoamine oxidase.
Pharmaceutics:
Preparations are available for ophthalmic, nasal, subcutaneous, intramuscular or
intravenous administration.
Subcutaneous and intramuscular injections have an onset of 10-15 min and
remain effective upto 1 and 2 hrs respectively. On intravenous administration the onset of
37
action is immediate with peak effect at 2-5 minutes and lasts for 15-20 minutes. The
elimination half life of phenylephrine is about 2.5 to 3 hours.
Parenteral forms: 1% injection containing phenylephrine hydrochloride 10mg/ml
ampoules. The injections are intended for subcutaneous, intramuscular or slow
intravenous injection, or intravenous infusion.
For intravenous injection, the injection may be diluted to a concentration of 0.1%
phenylephrine hydrochloride (1mg/ml) with sterile water for injection.
For intravenous infusion, 1ml of the phenylephrine hydrochloride injection
(10mg/ml) is diluted with 500ml 5% dextrose or 0.9% sodium chloride intravenous
infusions.
Generally, phenylephrine hydrochloride preparations should be protected from
light.
Therapeutic Use:
Indications:
1. Topical vasoconstrictor effects- nasal decongestant
2. Mydriasis
3. Pressor action
4. Paroxysmal supraventricular tachycardia
5. Adjunct to local anaesthesia for its vasoconstrictor action
6. As acid tartarate to prolong the bronchodilator effect of isoprenaline used as inhaler
7. Fecal incontinence and priapism
38
Contraindications:
Absolute contraindication: Concurrent administration of monoamine oxidase inhibitors
Relative contraindications:
1. Tricyclic antidepressants
2. Hypertension
3. Unstable angina and recent myocardial infarction
4. Hyperthyroidism
Aneasthetic uses:
Pressor actions:
It is weaker than that of noradrenaline but of longer duration
The pressor effect of phenylephrine is useful in anaesthesia and intensive care. It
is preferred over other agents to produce vasoconstriction, since it has little β1
adrenoreceptor activity, and hence is less prone to producing dysrythrmias or
chronotropic side effects. It may be associated with alterations in left ventricular filling
dynamics, and transient impairment of global left ventricular wall stress. It is preferred
over methoxamine because of shorter duration of action, 5-10 min versus 30-60min.
Subcutaneous or intramuscular: 2-5mg upto 10mg. initial dose should not exceed 5mg
Intravenous- 0.2mg (0.1-0.5mg) Initial dose should not exceed 0.5mg. Injections
should not be repeated more often than every 10-15 minutes
continuous infusion: 10mg phenylephrine in 500ml of 5% dextrose or 0.9% sodium
chloride(20µg/ml) infused initially t a rate of upto 180µg/min, reduced according to
response to 30-60µg/min
39
General anaesthesia:
The vasodilating properties of general anesthetics can be overcome by judicious
use of intravenous phenylephrine.
If during the usage of venous or arterial dilators, excessive falls in blood pressure
are encountered, these can be reversed by phenylephrine.
It has been used to improve the intraoperative blood pressure following surgical
removal of pheochromocytoma, following removal of an aortic cross clamp, and during
cardiopulmonary bypass and carotid artery surgery to maintain cerebral perfusion.
Regional anaesthesia:
Hypotension following spinal and epidural anaesthesia is primarily caused by
peripheral vasodilation and responds to phenylephrine.
Sepsis:
It has beneficial effect on hemodynamic and oxygen transport variables, on
hyperlactemia, and renal function, following volume resuscitation in patients with
hyperdynamic sepsis. Infusion rates of 10mg/hr may be necessary.
Initial dose of 2-5mg as 1% solution subcutaneous or intramuscular with further
doses of 1mg to 10mg if necessary.100-500µg by slow intravenous. injection as 0.1%
solution repeated as necessary after at least 15min.
In severe cases- 0.1% solution initially at a rate of not more than 180µg/min,
reduced according to response to 30-60µg/min
Paroxysmal supraventricular tachycardia: rapid intravenous injections are required.
Initial dose of 0.5mg followed by 0.1 to 0.2 mg subsequently but not more than 1mg.
Cardiopulmonary resuscitation:
It may improve the outcome.
40
Adverse reactions:
1. Potentially life threatening effect: Persistent or severe hypertension complicated
by headache, vomiting, and profound reflex bradycardia. Infants and children
appear to be at risk.
2. Acute overdosage: clinical features are a rise in blood pressure with reflex
bradycardia which can be countered by intravenous infusion of phentolamine.
3. Severe irreversible adverse effects: severe tissue necrosis if injected other than
intravenously
4. Symptomatic adverse effects: local application to conjunctiva may cause stinging
5. Other effects: interferes with potassium movement into the cells during acute
potassium administration , although there is no effect on serum potassium
High risk group:
1. Neonates
2. Children
3. Elderly
4. Concurrent disease – IHD , chronic pulmonary hypertension and right ventricular
failure
Drug interactions: severe hypertension may occur when given concurrently with
antidepressants of monoamine oxidase and tricyclic types, ganglion blocking agents,
adrenergic blocking agents, rauwolfia alkaloids and methyldopa.
41
REVIEW OF CLINICAL STUDIES
Joupilla and colleagues (1984)26conducted a study on Subarachnoid blockade
using 0.5% bupivacine after a “preload“ of Ringer's lactate solution 1500–2000 ml
intravenous. in nine patients undergoing elective Caesarean section. ephedrine infusion
50 mg in 500 ml was instituted at the first signs of maternal hypotension in seven
patients. Although significant decreases in mean maternal systolic, mean and diastolic
arterial pressures were recorded, the individual decreases in pressure were less than 30
mm Hg in all except two patients. In general placental blood flow did not change,
although there was a marked increase in one patient with toxaemia and a decrease in one
woman with diabetes mellitus. The babies were unaffected at delivery. Preventive
measures, especially the “preload” infusion, are important in the maintenance of adequate
placental perfusion in patients undergoing Caesarean section under subarachnoid
blockade.
Bhagwanjee S and others (1990)27 conducted a study on Prevention of
Hypotension Following Spinal Anaesthesia for Elective Caesarean Section by Wrapping
of the Legs. Twenty-four parturients undergoing elective Caesarean section were
allocated randomly to have the legs wrapped with elasticated Esmarch bandages
immediately following spinal anaesthesia or to serve as controls. Significant hypotension
(systolic arterial pressure < 100 mm Hg and < 80% of baseline value) was treated with i.
v. ephedrine in 5-mg boluses. Leg wrapped patients had a significantly lower incidence
(16.7%) of hypotension than controls (83.3%). Only two patients in the leg wrapped
group required ephedrine compared with 10 in the control group. Systolic arterial
42
pressure was significantly less in control subjects at 4, 5 and 6 min following spinal
injection. No patient in the leg wrapped group became hypotensive following removal of
the elasticated bandages.
Moran DH and colleagues (1991)28 conducted a study on phenylephrine in the
prevention of hypotension following spinal anaesthesia for cesarean delivery. It was a
randomized double blinded study. Patients were randomly assigned to receive either
ephedrine (n = 29) in 10 mg intravenous bolus injections or phenylephrine (n = 31) in 80
µg intravenous bolus injections to maintain systolic blood pressure (SBP) above 100 mm
Hg. Maternal venous, umbilical artery, and umbilical vein blood gases were measured,
and neonatal APGAR scores and Early Neonatal Neurobehavior Scale scores were
assessed. It was observed that phenylephrine is as effective as ephedrine in the treatment
of maternal hypotension, and when used in small incremental bolus injections, it appears
to have no adverse neonatal effects in healthy, nonlaboring parturients.
Robson SC and colleagues (1992)29 conducted a study on Maternal and fetal
haemodynamic effects of spinal and extradural anaesthesia for elective caesarean section.
Serial haemodynamic investigations were performed in 32 women who were allocated
randomly to receive either spinal or extradural anaesthesia for elective Caesarean section.
Cardiac output was measured by Doppler and cross-sectional echo-cardiography at the
aortic valve. Doppler flow velocity waveforms were recorded also from the umbilical
artery. Preloading with Ringer lactate solution 1 liter increased cardiac output in both
groups. After injection of bupivacaine, cardiac output remained increased in the
extradural group, but decreased in the spinal group. This was associated with an increase
in umbilical artery pulsatility index in the spinal group. Umbilical artery pH was less in
43
the spinal group (7.22 vs 7.27), although no neonate was depressed at birth. The
maximum percentage change in cardiac output and umbilical artery pulsatility index
correlated with umbilical artery pH (r = 0.54, r = 0.72, respectively). There was no
significant correlation with change in arterial pressure.
Rout CC, Rocke DA. and Gouws E (1993)30 conducted a study on Leg elevation
and wrapping in the prevention of hypotension following spinal anaesthesia for elective
caesarean section. Ninety-seven parturients undergoing elective Caesarean section were
allocated randomly to have their legs elevated to approximately 30 degrees on pillows or
elevated and wrapped with elasticated Esmarch bandages or neither (controls) following
spinal anaesthesia. All patients received intravenous crystalloid (20 ml.kg-1 over 20 min)
prior to spinal injection and were placed in the left lateral tilt position. Significant
hypotension was treated with intravenous ephedrine in 5 mg bolus doses. Leg wrapping
resulted in a significant reduction in the incidence of postspinal hypotension in
comparison to the control group (18% compared to 53%). This represents a five-fold
reduction in the likelihood of postspinal hypotension (odds ratio 5.3, 95% CI 1.7-16.3).
Leg elevation alone did not significantly reduce the incidence of hypotension (39%).
There was no significant difference in the time of onset of hypotension between the
groups. For those patients requiring ephedrine, there was no significant difference in
mean dose requirements between the groups. The use of leg compression immediately
postspinal provides a simple means of reducing the accompanying hypotension and
should be used more widely.
44
Hall PA, Bennett A, Wilkes MP, Lewis M. (1994)31 conducted a study, Spinal
anaesthesia for caesarean section: comparison of infusions of phenylephrine and
ephedrine. Maternal cardiovascular changes and neonatal acid-base status were assessed
in 29 healthy women undergoing elective lower segment Caesarean section under spinal
anaesthesia. The patients were allocated randomly to one of three groups to receive an
intravenous. infusion of one of the following: ephedrine 1 mg min-1(E1), ephedrine 2 mg
min-1(E2), or phenylephrine 10 µg min-1(P). Invasive arterial pressure was monitored
continuously and if hypotension occurred (defined as a 20% decrease from baseline,
taken after intravenous. preload administration), bolus doses of either ephedrine or
phenylephrine were given. Only four patients became hypotensive in group E2, compared
with eight patients in group E1 and nine patients in group P. The total time that the
patients remained hypotensive was greatest in group P, less in group E1 and least in
group E2. Neonatal APGAR scores and acid-base profiles were similar in all three
groups. In this study, an infusion of phenylephrine 10 µg min-1 with bolus doses of 20 µg
was shown to be significantly less effective in maintaining systolic arterial pressure
within 20% limits of baseline compared with an infusion of ephedrine 1 or 2 mg min-1
with bolus doses of 6 mg.
Thomas DG and colleagues (1996)32 conducted a study on Randomized trial of
bolus phenylephrine or ephedrine for maintenance of arterial pressure during spinal
anaesthesia for Caesarean section. Thirty-eight healthy women undergoing elective
Caesarean section under spinal anaesthesia at term were allocated randomly to receive
boluses of either phenylephrine 100 µg or ephedrine 5 mg for maintenance of maternal
arterial pressure. The indication for administration of vasopressor was a reduction in
45
systolic pressure to < or = 90% of baseline values. Maternal arterial pressure (BP) and
heart rate (HR) were measured every minute by automated oscillometry. Cardiac output
(CO) was measured by cross-sectional and Doppler echocardiography before and after
preloading with 1500 ml Ringer lactate solution and then every 2 min after administration
of bupivacaine. Umbilical artery pulsatility index (PI) was measured using Doppler
before and after spinal anaesthesia. The median (range) number of boluses of
phenylephrine and ephedrine was similar. Maternal systolic BP and CO changes were
similar in both groups, but the mean maximum percentage change in maternal HR was
larger in the phenylephrine group than in the ephedrine group. As a consequence atropine
was required in 11/19 women in the phenylephrine group compared with 2/19 in the
ephedrine group. Mean umbilical artery pH was higher in the phenylephrine group than
in the ephedrine group. The results of the present study support the use of phenylephrine
for maintenance of maternal arterial pressure during spinal anaesthesia for elective
Caesarean section.
Nagan kee WD, Khaw KS, Lee BB, Ng FF and Wong MMS (2001)33
conducted a Randomized controlled study of colloid preload before spinal anaesthesia
for Caesarean section. They randomized women having elective Caesarean section to
receive either no preload (control group, n=33) or 4% gelatin solution (Gelofusine)
15 ml kg–1 (colloid group, n=35) intravenous before spinal anaesthesia. Intravenous
metaraminol was titrated at 0.25–0.75 mg min–1 to maintain systolic arterial pressure
(SAP) in the target range 90–100% of baseline after the spinal injection. The control
group required more vasopressor in the first 10 min [median 1.7 (range 0–2.9) mg vs 1.4
(0–2.8)] at a greater maximum infusion rate [0.5 (0–0.75) vs 0.25 (0–0.5) mg min–1] and
46
had a lower minimum SAP [90 (51–109) vs 101 (75–127) mm Hg] than the colloid
group. Nausea was less frequent in the colloid group (6 vs 24%) but neonatal outcome
was similar in the two groups. Colloid preload improved haemodynamic stability but did
not affect neonatal outcome when arterial pressure was maintained with an infusion of
metaraminol during spinal anaesthesia for Caesarean section.
Mercier FJ and coworkers (2001)34conducted a study on phenylephrine added
to prophylactic ephedrine infusion during spinal anaesthesia for elective cesarean section.
It was a randomized double blinded study. A vasopressor infusion was started
immediately after spinal injection of either 2 mg/min ephedrine plus 10 µg/min
phenylephrine or 2 mg/min ephedrine alone. The infusion rate was adjusted according to
systolic blood pressure using a predefined algorithm. Hypotension was treated with 6 mg
ephedrine bolus doses. Hypotension occurred less frequently in the ephedrine-
phenylephrine group than in the ephedrine-alone group. Median supplemental ephedrine
requirements and nausea scores were less in the ephedrine-phenylephrine group.
Umbilical artery pH values were significantly higher in the ephedrine-phenylephrine
group than in the group that received ephedrine alone. APGAR scores were similarly
good in both groups. It was concluded that phenylephrine added to an infusion of
ephedrine halved the incidence of hypotension and increased umbilical cord pH.
Ayorinde BT and colleagues (2001)35 conducted a study on evaluation of
pre‐emptive intramuscular phenylephrine and ephedrine for reduction of spinal
anaesthesia‐induced hypotension during Caesarean section. Pre‐emptive intramuscular
vasopressors were evaluated in 108 patients undergoing elective Caesarean section under
spinal anaesthesia, assigned to four groups in a randomized, double‐blind,
47
placebo‐controlled study. Group I received pre‐emptive phenylephrine 4 mg
intramuscular, group II received phenylephrine 2 mg intramuscular, group 3 received
ephedrine 45 mg intramuscular, while controls received an intramuscular injection of
saline, all given immediately after induction of spinal anaesthesia. Rescue intravenous
boluses of ephedrine were given if the patient was hypotensive or reported nausea,
vomiting or dizziness. The incidence of hypotension was 33% in the phenylephrine 4 mg
group compared with 70% in the control and phenylephrine 2 mg groups, and 48% in the
ephedrine 45 mg group. The phenylephrine 4 mg and ephedrine 45 mg groups had a
significantly lower percentage reduction in MAP compared with controls. They also had
a lower total dose of rescue intravenous ephedrine mg and compared with controls. It was
concluded that pre‐emptive intramuscular phenylephrine 4 mg and ephedrine 45 mg
reduce the severity of hypotension and the total dose of rescue intravenous ephedrine
during spinal anaesthesia for Caesarean section.
Ngan Kee WD, Lau TK, Khaw KS, Lee BB (2001)36 conducted a study on
metaraminol Infusion for Maintenance of Arterial Blood Pressure during Spinal
Anaesthesia for Cesarean Delivery: The Effect of a Crystalloid Bolus. They randomly
allocated women having elective cesarean delivery to receive either no bolus or 20 mL/kg
lactated Ringer’s solution intravenous before spinal anaesthesia. An infusion of
metaraminol started at 0.25 mg/min was titrated to maintain systolic arterial blood
pressure in the target range 90%–100% of baseline. The total dose of metaraminol
required up to the time of uterine incision was similar between the Control Group and the
Bolus Group. However, the Control Group required more metaraminol in the first 5 min
and a faster maximum infusion compared with the Bolus Group. There was no difference
48
between groups in regards to changes in systolic arterial blood pressure or heart rate over
time, or maternal or neonatal outcome. It was concluded that when metaraminol is used
to maintain arterial pressure during spinal anaesthesia for cesarean delivery, crystalloid
bolus is not essential provided that sufficient vasopressor is given in the immediate
postspinal period.
Cooper DW and colleagues (2002)37 conducted a study on fetal and maternal
effects of phenylephrine and ephedrine during spinal anaesthesia for cesarean delivery.
The study was randomized and double blinded. It compared phenylephrine 100 µg/ml
(phenylephrine group), ephedrine 3 mg/ml (ephedrine group), and phenylephrine 50
µg/ml combined with ephedrine 1.5 mg/ml (combination group), given by infusion, to
maintain maternal systolic arterial pressure at baseline during spinal anaesthesia for
elective cesarean delivery. Fetal acidosis was less frequent in the phenylephrine group
and less frequent in the combination group than in the ephedrine group. The mean
systolic arterial pressure was similar for the three groups. The mean heart rate was higher
in the ephedrine group than in the phenylephrine group, or the combination group).
Nausea and vomiting were less frequent in the phenylephrine group than in the ephedrine
group or the combination group. It was concluded that giving phenylephrine alone by
infusion at cesarean delivery was associated with a lower incidence of fetal acidosis and
maternal nausea and vomiting than giving ephedrine alone. There was no advantage to
combining phenylephrine and ephedrine because it increased nausea and vomiting, and it
did not further improve fetal blood gas values, compared with giving phenylephrine
alone.
49
Loughrey JP and coworkers (2005)38 did a study on Hemodynamic effects of
spinal anaesthesia and simultaneous intravenous bolus of combined phenylephrine and
ephedrine versus ephedrine for cesarean delivery. Forty-three term parturients were
randomized to receive a bolus of ephedrine 10 mg ± phenylephrine 40 µg (groups E and
EP, respectively) simultaneously with spinal anaesthesia. Hypotension was defined as a
systolic blood pressure below 100 mm Hg or a decrease of 20% from a baseline value.
Rescue boluses comprised of ephedrine 5 mg ± phenylephrine 20 µg. It was observed that
the incidence of hypotension was 80% in patients receiving ephedrine and was 95% in
patient receiving ephedrine with phenylephrine. It was concluded that the combination of
ephedrine and phenylephrine given as an intravenous bolus at the doses selected is not
superior to ephedrine alone in preventing or treating hypotension in healthy parturients
undergoing cesarean delivery.
Ngan Kee and colleagues (2005)39 did a study on Prevention of Hypotension
during Spinal Anaesthesia for Cesarean Delivery - An Effective Technique Using
Combination phenylephrine Infusion and Crystalloid Cohydration. Nonlaboring patients
scheduled to undergo elective cesarean delivery received an intravenous infusion of
100µg/min phenylephrine that was started immediately after spinal injection and titrated
to maintain systolic blood pressure near baseline values until uterine incision. In addition,
patients received infusion of lactated Ringer's solution that was given either rapidly
(group I, n = 57) or at a minimal maintenance rate (group 0, n =55). Maternal
hemodynamic changes and neonatal condition were compared. The incidence of
hypotension was greater in group 0 than group I. Total phenylephrine consumption was
smaller in group I compared with group 0 (P = 0.008). Neonatal outcome and maternal
50
side effects were similar between groups. It was concluded that Combination of a high-
dose phenylephrine infusion and rapid crystalloid cohydration is the first technique to be
described that is effective for preventing hypotension during spinal anaesthesia for
cesarean delivery
Sarvanan S and coworkers (2005)40 did a study on equivalent dose of ephedrine
and phenylephrine in the prevention of post-spinal hypotension in Caesarean section.
Patients were randomized into 2 groups The first patient in Group A received 50 mg of
ephedrine in saline 0.9% w/v, 500 ml, at 999 ml h–1, the maximum rate possible on the
pump and the first patient in Group B received 500 µg of phenylephrine in saline 0.9%
w/v, 500 ml, at the same rate. The initial dose for dilution was an arbitrary choice. The
dose of vasopressor in the saline bag for every subsequent patient was established by the
efficacy of the dose in preventing hypotension in the previous patient according to the
technique of up–down sequential allocation. Minimum vasopressor dose for each drug
was determined according to the Dixon–Massey formula. The minimum vasopressor dose
in saline 500 ml was 532.9 µg (95% CI 506.0–559.8) for phenylephrine and 43.3 mg
(95% CI 39.2–47.3) for ephedrine. The concentration needed for equivalence at an
infusion rate of 999 ml h–1 was 1.07µg ml–1 for phenylephrine and 86.66 µg ml–1 for
ephedrine. This study demonstrates a potency ratio of 81.2 (95% CI 73.0–89.7) for
equivalence between phenylephrine and ephedrine in prevention of hypotension after
spinal anaesthesia for Caesarean section.
Sharma R, Maitra N and Niyogi M (2005)41 compared bolus phenylephrine and
mephentermine for Treatment of Hypotension during Spinal Anaesthesia for Cesarean
Section. The participants were randomly allocated either bolus phenylephrine 100 µg or
51
mephentermine 6 mg upon developing hypotension. The volume of each dose was
equaled by adding 0.9% NaCl solution making the concentration of mephentermine 6
mg/mL and that of phenylephrine 100 µg/mL The identical syringes containing the
solution were unlabeled and put in labeled tray. This study shows that both vasopressors
can be used for the indication. The clinical outcomes like neonatal APGAR score,
incidence of nausea and vomiting and other adverse events were comparable with both
the vasopressors. phenylephrine however had the advantage of decreased heart rate and
requirement of lesser amount and more efficacy at maintaining the arterial blood
pressure. The systolic blood pressure was significantly higher with phenylephrine 6
minutes after administration as compared to mephentermine. They concluded that
mephentermine should be avoided in patients in whom increased heart rate may be
undesired. phenylephrine seems to be a better choice for the treatment of hypotension
during spinal anaesthesia for cesarean section.
Ngan Kee WD and coworkers (2007)42 conducted a randomized double-blinded
comparison of phenylephrine and ephedrine infusion combinations to maintain blood
pressure during spinal anaesthesia for cesarean delivery: the effects on fetal acid-base
status and hemodynamic control. Patients received intravenous infusion of
phenylephrinre and ephedrine combined in one of five different concentration ratios.
Assuming phenylephrine 100µg equipotent to ephedrine 8mg, the groups contained the
proportional potency equivalent of 100%, 75%, 50%, 25% or 0% of phenylephrine and
0%, 25%, 50%, 75% or 100%, respectively, of ephedrine. The infusions were adjusted to
maintain systolic blood pressure (SBP) near baseline until uterine incision. Hemodynamic
changes and umbilical cord blood gases were compared. Hemodynamic changes and
52
umbilical cord blood gases were compared. It was observed that as the proportion of
phenylephrine decreased and proportion of ephedrine increased among the groups the
incidences of hypotension and nausea/vomiting increased, the median magnitude of
deviations of SBP above or below baseline and the bias for SBP to be above baseline
increased, maternal heart rate was faster, fetal pH and base excess decreased, umbilical
arterial oxygen content decreased and umbilical venous PO2 increased. When varying
combinations of phenylephrine and ephedrine were given by infusion to maintain arterial
blood pressure during spinal anaesthesia for cesarean delivery, as the proportion of
phenylephrine decreased and the proportion of ephedrine increased, hemodynamic
control was reduced and fetal acid-base status was less favorable. Combinations of
phenylephrine and ephedrine appear to have no advantage compared with phenylephrine
alone when administered by infusion for the prevention of hypotension associated with
spinal anaesthesia for cesarean delivery.
Prakash S and colleagues (2009)43conducted a study on Maternal and neonatal
effects of bolus administration of ephedrine and phenylephrine during spinal anaesthesia
for caesarean delivery: a randomised study. It was a double-blind study. Women received
boluses of either ephedrine 6 mg or phenylephrine 100 µg whenever maternal systolic
pressure was 80% of baseline. Changes in systolic pressure were comparable in the two
groups. There were no differences in the incidence of bradycardia, nausea and vomiting
.Umbilical artery (UA) pH and venous pH were significantly greater in group P than in
group E. UA base excess was significantly less in group E than in group P. APGAR
scores at 1, 5 and 10min and neurobehavioural scores at 2-4 h, 24 h and 48 h were similar
in the two groups. It was concluded that phenylephrine 100 µg and ephedrine 6 mg had
53
similar efficacy in the treatment of maternal hypotension during spinal anaesthesia for
elective caesarean delivery. Neonates in group P had significantly higher umbilical
arterial pH and base excess values than those in group E, which is consistent with other
studies.
Dyer RA and colleagues (2009)44 conducted a study on Hemodynamic effects of
ephedrine, phenylephrine, and the coadministration of phenylephrine with oxytocin
during spinal anaesthesia for elective cesarean delivery. Forty-three patients were
randomized to receive 80 µg of phenylephrine or 10 mg of ephedrine. Both pulse wave
form analysis and transthoracic bioimpedance changes were used to estimate stroke
volume in each patient. Hemodynamic responses to spinal anaesthesia and oxytocin were
also recorded. A subgroup of 20 patients was randomized to receive oxytocin compared
with oxytocin plus 80 µg of phenylephrine after delivery. Mean CO and maximum
absolute response in CO were significantly lower during the 150seconds after
phenylephrine administration than after ephedrine. CO changes correlated with heart rate
changes. Coadministration of phenylephrine obtunded oxytocin-induced decreases in
systemic vascular resistance and increases in heart rate and CO. Trends in CO change
were similar using either monitor. It was concluded that Bolus phenylephrine reduced
maternal CO, and decreased CO when compared with ephedrine during elective spinal
anaesthesia for Cesarean delivery. CO changes correlated with heart rate changes after
vasopressor administration, emphasizing the importance of heart rate as a surrogate
indicator of CO. Coadministered phenylephrine obtunded hemodynamic responses to
oxytocin.
54
Ngan Kee WD and colleagues (2009)45 conducted a study on Placental Transfer
and Fetal Metabolic Effects of phenylephrine and ephedrine during Spinal Anaesthesia
for Cesarean Delivery. A total of 104 women having elective Cesarean delivery under
spinal anaesthesia randomly received infusion of phenylephrine (100µg/ml) or ephedrine
(8 mg/ml) titrated to maintain systolic blood pressure near baseline. At delivery, maternal
arterial, umbilical arterial, and umbilical venous blood samples were taken for
measurement of blood gases and plasma concentrations of phenylephrine, ephedrine,
lactate, glucose, epinephrine, and norepinephrine. In the ephedrine group, umbilical
arterial and umbilical venous pH and base excess were lower, whereas umbilical arterial
and umbilical venous plasma concentrations of lactate, glucose, epinephrine, and
norepinephrine were greater. Umbilical arterial PCO2 and umbilical venous PO2,
Placental transfer, the umbilical arterial/umbilical venous plasma concentration ratio was
greater for ephedrine. It was concluded that ephedrine crosses the placenta to a greater
extent and undergoes less early metabolism and/or redistribution in the fetus compared
with phenylephrine. The associated increased fetal concentrations of lactate, glucose, and
catecholamines support the hypothesis that depression of fetal pH and base excess with
ephedrine is related to metabolic effects secondary to stimulation of fetal β-adrenergic
receptors. Despite historical evidence suggesting uteroplacental blood flow may be better
maintained with ephedrine, the overall effect of the vasopressors on fetal oxygen supply
and demand balance may favor phenylephrine
Pinto V, Jaysundara N, Abeysundara A, Ekanayake S (2009)46 conducted a
study on the use of phenylephrine as vasopressor of choice to prevent hypotension
following spinal anaesthesia in LSCS. Two groups were identified as case and control
55
and the sample size was 30 from each category. Cases received intravenous infusion of
phenylephrine 20-40ml/hr (100µg/ml) and it was started immediately after spinal
injection and titrated to maintain systolic blood pressure near baseline value. Controls
were given ephedrine 5mg boluses with the evidence of drop of blood pressure only. The
data included the blood pressure, heart rate, ECG changes, maternal complaints, data to
asses the staff satisfaction and also to asses the manuverbility of use of phenylephrine in
the OT setup. In ephedrine group 79.16% showed drop of blood pressure which needed
ephedrine boluses, in contrast to 10% in the phenylephrine group. Fetal out come in both
groups were more or less the same. In ephedrine group there were no complaints from
30% (9) of mothers. 43.33% (13) complained of having headache during the procedure
and 26.66% (8) complained of nausea and vomiting during the proedure. (Z=1.96). In
phenylephrine group there were no complaints from 90% of mothers and only 10%
complained of having headache during the procedure. Proportionately high ranking with
the OT staff regarding the manuverbility of phenylephrine infusion was seen. It was
concluded that phenylephrine is a better alternative vasopressor for spinal induced
hypotension.
56
METHODOLOGY
Source of data
Patients posted for elective cesarean section under spinal anaesthesia in
A.J.Institute of medical sciences.
Approval and Consent
This study was undertaken after obtaining approval of the Hospital Ethics
committee and written informed consent from the patients.
Preoperative Protocol
All the patients were evaluated on the previous day. The procedure was explained
to the patient and possible complication associated with the procedure was explained to
the patient in their mother tongue. A written informed consent was obtained. The patients
were asked to maintain NPO status for 8 hours preoperatively.
Investigation required
1. Hb% , TC, DC
2. HIV , HBsAg
3. RBS, Blood Urea , Serum Creatinine
4. Urine analysis
5. ECG
Method of collection of data
This is a randomized controlled study performed over a period of one year from
November 2009 to November 2010. The study was carried out on 50 patients between the
57
age group of 20-35 years belonging to American society of Anesthesiologist (ASA) grade
II who were scheduled for elective Caesarean section during the study period under
spinal anaesthesia.
Patients were allotted into 2 groups on basis of random sampling method.
In Group I the patients received intravenous prophylactic phenylephrine infusion
at 100µg/min for 3min after completion of intrathecal injection. Then each min SAP was
measured and infusion stopped if SAP> baseline and continued or restarted if less than or
equal to baseline SAP. Intravenous phenylephrine bolus 100µg was given when SAP is
decreased to <80% of baseline.
In Group II- the patients received intravenous phenylephrine bolus 100µg when
SAP is decreased to <80% of baseline
Inclusion criteria:
Singleton full term pregnant patients, age 20- 35yrs of ASA grade II scheduled for
elective caesarean section under spinal anaesthesia
Exclusion criteria:
Patients above 35yrs
Patients below 20 yrs
Patients having resting blood pressure >140/90mm Hg , history of hypertension ,
preeclampsia / eclampsia, hyperthyroidism
Patients having co- existing neurological , cerebrovascular , cardiovascular, renal,
metabolic, psychiatric disorder
Patients with glaucoma, occlusive vascular disorder
58
History of hypersensitivity to local anesthetics and any contraindications to spinal
anaesthesia or having known fetal abnormalities
Fetal distress
Parameters to be studied:
Heart rate, Systolic and diastolic blood pressure every minute after induction of
spinal anaesthesia up to the extraction of the baby.
Incidence of hemodynamic adverse effects
Incidence of nausea and vomiting
Umbilical artery blood pH
APGAR score at 1 and 5 minutes
METHOD
Premedication
All parturients were premedicated with injection ranitidine 50mg intravenously
one hour before surgery.
Procedure
After premedication Patients were allowed to rest undisturbed for several minutes,
during which SAP was measured every 1–2 min. This was continued until measurements
became consistent. Baseline SAP, DAP and HR were taken as the mean of the two
recordings. After receiving the patient inside the operation theatre, baseline vital signs
were recorded using Multiparameter Monitor. Patients were preloaded with ringer lactate
59
solution, 10ml/kg over 15minutes after securing intravenous line with 18 gauze cannula
and continued at 10 mL/min.
Spinal anaesthesia was induced with patients in the lateral position. After skin
infiltration with lidocaine, a 23-gauge Quinche babcocks needle was inserted at the L2-3
or L3-4 vertebral interspace, and hyperbaric 0.5% bupivacaine 2.0 mL was injected
intrathecally. Patients were then immediately turned supine with left uterine displacement
with the help of a wedge. SAP was measured at 1-min intervals beginning 1 min after
spinal injection.
Immediately after the completion of intrathecal injection, phenylephrine infusion
was started in group I patients at 1 mL/min (100 µg/min), whereas patients in the control
group did not have it. Infusions were administered with a syringe pump that was
connected to the intravenous line via a three-way stopcock and were continued for a
minimum of 3 min, after which the infusion was either stopped or continued according to
protocol based on the SAP measurement at each minute. After each 1-min measurement
of SAP, the infusion was stopped if the SAP was more than baseline, and it was
continued or restarted if the SAP was less than or equal to baseline. For the purposes of
the study, we defined hypotension as a decrease in SAP to <80% of baseline. Each time
there was a SAP measurement showing hypotension, patients received a 100 µg
intravenous bolus of phenylephrine both in group I and group II. The dosing regimens for
phenylephrine were selected on the basis of previous studies.
Oxygen was routinely given at 4 L/min by clear face mask. Any incidences of
nausea (reported by patients) or vomiting (observed by investigators) were recorded. We
planned to treat nausea or vomiting that was not associated with hypotension with
60
intravenous ondansetron 8mg and to treat bradycardia, defined by an HR <50 bpm with
intravenous atropine 0.6mg.
After intrathecal injection of local anesthetic bupivacaine, the upper sensory level
of anaesthesia was measured by assessing loss of pinprick discrimination. Further checks
of the block height were made as required before the start of surgery, but these levels
were not recorded as part of the study. After 1 minute of SAB; HR, SAP and DBP were
recorded every minute till the extraction of the baby. The dosing regimens for
phenylephrine were selected on the basis of previous studies. The times of skin incision,
uterine incision, and delivery were recorded. The infusion and bolus protocol was
continued until the time of delivery of the baby, after which further management was at
the discretion of the attending anesthesiologist, who was free to administer intravenous
fluids and vasopressors as appropriate to replace surgical losses and maintain SAP. The
total volumes of study solutions given up to the time of delivery of the baby were
recorded.
After delivery, oxytocin 20 IU in 1000ml saline was given by slow intravenous
infusion. APGAR scores were assessed 1 and 5 min after delivery. Umbilical artery blood
samples were taken from a double-clamped segment of umbilical cord by for immediate
blood gas analysis.
Statistical analysis:
The observations are expressed as Mean ± standard deviation. The baseline
haemodynamic values and the postspinal haemodynamic changes at various time
intervals were compared using unpaired “t” test. Mann whitney test, Chi-square and
61
Fisher Exact test has been used to find the significance of study parameters as
appropriate. Significance is assessed at 5% level of significance.
The statistical significance of the difference between group I and group II were
based on P value.
A ‘P’ value of <0.05 was considered to be statistically significant
P<0.01 was considered to be highly significant
P<0.001 was considered to be very highly significant
P>0.05 was considered to be not significant
62
RESULTS AND ANALYSIS
MATERNAL CHARACTERISTICS: Age, weight, and height characteristics of two
groups in our study series were comparable as shown in Table 2 and graph Numbers 1a,
1b and 1c.
Table No. 2: Comparison of basic parameters between two groups
Basic characteristics
Group I Group II P value t value
Age 25.84 ± 2.89 25.04 ± 2.28 0.2855 1.08
Weight 64.20±5.63 64.88±2.33 0.5794 0.558
Height 157.72±4.83 155.68±2.64 0.0705 1.85
V
AG
E (Y
EAR
S)
GROUP 1 GROUP 210
20
30
40
Graph No. 1(a): Showing age distribution
63
V
HEI
GH
T (C
MS)
GROUP 1 GROUP 2140
150
160
170
Graph No. 1(b): Showing height distribution
V
WEI
GH
T (K
gs)
GROUP 1 GROUP 250
60
70
80
Graph No. 1(c): Showing weight distribution
64
The age of the patients ranged from 20-30 years. The mean age in group I was
25.8400 (SD 2.89) years, in group II was 25.04 (SD 2.28) years.
The weight of the patients ranged from 55-75 kgs. The mean weight in group I
was 64.20 (SD 5.63), in group II was 64.88 (SD 2.33) kg.
The height of the patients ranged from 150-168cms. The mean height in group I
was 157.72 (SD4.83), in group II was 155. 68 (SD 2.64) cm.
Hence, age, weight and height were comparable in all the two groups and were
found to be statistically insignificant.
65
LEVEL OF BLOCKADE: The level of sensory block obtained is also comparable in
both the groups and most of the patients had average blockade level of T6.
Table No. 3: Comparison of sensory levels between two groups
Level of Blockade Group I Group II
T4 6 (24%) 7 (28%)
T5 5 (20%) 6(24%)
T6 14 (56%) 12(48%)
X2=0.322 P value= 0.8238
Graph No. 2: Level of sensory blockade
66
MATERNAL HEART RATE VARIATIONS: The ranges of mean maternal heart rates
in group I, group II were 86.96 -95.00 bpm, 90.08-95.00 respectively. The heart rate was
significantly lower in the infusion group in the 1st, 2nd, 10th and 11th minute.
Table No. 4: Comparison of HR between two groups of patients
Study period
Group I
Group II P value t value
Mean SD Mean SD
bhr 90.6400 7.14656 92.3200 3.77183 0.304 1.03900
1 min 89.3600 7.82560 94.4000 5.14782 0.01 2.69000
2 min 89.7600 7.55690 94.1600 5.79281 0.025 2.31100
3 min 90.4400 6.89251 91.3200 4.67012 0.61 .52800
4 min 88.8000 7.25718 91.1600 3.84794 0.152 1.43700
5 min 88.2000 5.67891 90.3200 6.28967 0.217 1.25100
6 min 86.9600 7.12086 90.0800 4.60905 0.072 1.83900
7 min 88.1600 6.49153 90.4800 3.52515 0.125 1.57000
8 min 87.6400 6.74463 90.9600 5.67509 0.066 1.88300
9 min 87.4783 8.52733 91.4167 6.06427 0.077 1.81800
10 min 87.0588 8.19657 93.3158 5.91657 0.012 2.64700
11 min 87.5000 5.68038 94.6364 2.41962 <0.001 3.91100
12 min 93.0000 4.08248 94.0000 2.00000 0.4121 -0.818
13 min 95.5000 3.53553 95.0000 - 0.8741 0.200
67
TIME (MINUTES)
HE
ART
RAT
E (b
pm)
baselin
e 1 2 3 4 5 6 7 8 9 10 11 12 13
70
80
90
100
110 Group 1
Group 2
Graph No. 3: Comparison of heart rate among two groups
68
SYSTOLIC BLOOD PRESSURE VARIATIONS: The variations in mean systolic
blood pressure in group I, group II after SAB were in the range of 123.00- 128.47 mm Hg
and 98.44-126.84 mm Hg respectively.
Table No. 5: Comparison of SBP (mm Hg) between two groups
Study period
Group I
Group II P value
t value
Mean SD Mean SD
BSBP 123.3600 8.58235 124.2400 6.67882 .688 -.405
1 min 125.2000 8.18026 126.8400 9.89815 .526 -.639
2 min 123.8400 10.07340 116.8400 13.00538 .039 2.128
3 min 125.5200 7.78417 103.0800 12.87413 .000 7.458
4 min 124.4000 7.92675 98.4400 10.63046 .000 9.788
5 min 124.4000 9.90791 101.0000 10.88577 .000 7.949
6 min 123.3200 10.72272 103.6800 8.81627 .000 7.074
7 min 126.2800 9.87218 108.3200 8.77363 .000 6.799
8 min 125.9200 6.74463 109.5200 8.79924 .000 6.406
9 min 125.3182 11.38665 109.3333 7.08131 .000 5.770
10 min 128.4706 4.73178 109.7895 9.36055 .000 7.417
11 min 128.4000 6.80126 110.0000 8.63713 .000 6.083
12 min 127.0000 8.98146 109.4000 7.79744 .005 3.525
13 min 123.0000 4.24264 100.0000 - .141 4.426
69
TIME (MINUTES)
SYST
OLI
C B
LOO
D P
RES
SUR
E (m
mH
g)
BASELINE 1 2 3 4 5 6 7 8 9 10 11 12 13
60
80
100
120
140Group 1
Group 2
Graph No. 4: Comparison of SBP among two groups
Both the groups had similar preinduction SBP; however, after SAB the mean
systolic blood pressure was higher in the infusion group and was statistically significant.
70
DIASTOLIC BLOOD PRESSURE VARIATIONS: The variations in mean diastolic
blood pressure in group I, group II after SAB were in the range of 72.7600-81.0000 mm
Hg and 63.4800- 74.2400 mm Hg respectively
Table No. 6: Comparison of DBP (mm Hg) between two groups
Study period
Group I
Group II P value t value
Mean SD Mean SD bdbp 74.5200 4.69148 72.2800 4.37340 0.087 1.75
1 min 75.4800 6.47508 74.2400 5.87566 0.4605 0.709
2 min 74.2400 6.58458 71.7200 5.87026 0.1628 1.43
3 min 74.6400 5.36097 67.4800 6.15169 <0.0001 4.39
4 min 73.8000 8.54888 65.4000 6.87386 0.0004 3.83
5 min 73.6400 7.89979 63.4800 14.19542 0.0031 3.13
6 min 72.7600 8.08435 67.0400 5.55638 0.0048 2.92
7 min 72.8800 6.99595 69.0000 6.95821 0.0537 1.97
8 min 73.8800 6.95414 68.7600 4.71946 0.0039 3.05
9 min 73.6522 8.13303 68.6250 3.92110 0.0069 2.72
10 min 75.5882 4.95049 67.8947 7.40041 0.0001 3.62
11 min 76.1333 5.54033 70.9091 3.14498 0.0101 2.80
12 min 78.2857 6.34335 70.0000 1.58114 0.0177 2.82
13 min 81.0000 2.82843 72.0000 - 0.1388 4.500
71
TIME (MINUTES)
DIA
ST
OL
IC B
LO
OD
PR
ESS
UR
E (m
mH
g)BASELIN
E 1 2 3 4 5 6 7 8 9 10 11 12 1340
50
60
70
80
90 Group 1
Group 2
Graph No. 5: Comparison of DBP among two groups
Both the groups had similar preinduction DBP; however, after SAB the mean
diastolic blood pressure was higher in the infusion group and was statistically significant.
72
MEAN BLOOD PRESSURE VARIATIONS: The variations in mean Mean blood
pressure in group I, group II after SAB were in the range of 89.6000 -95.0000 mm Hg,
76.4000-91.7600 mm Hg respectively
Table No. 7: Comparison of MBP ((mm Hg) between two groups
Study period
Group I
Group II P value
t value
Mean SD Mean SD
BMBP 90.8400 5.26530 89.6000 4.46281 .374 .898
1 min 92.0800 6.04097 91.7600 6.67258 .860 .178
2 min 90.7600 7.06093 86.7600 7.44580 .057 1.949
3 min 91.5600 5.32353 79.3200 7.98290 .000 6.378
4 min 90.6400 6.88525 76.4000 7.90569 .000 6.792
5 min 90.5600 8.15516 77.5600 8.05233 .000 5.672
6 min 89.6000 8.54400 79.2800 6.27508 .000 4.868
7 min 90.6800 7.20948 82.0400 6.69253 .000 4.392
8 min 91.1200 7.19560 82.4400 5.40894 .000 4.821
9 min 90.9130 8.60187 82.2917 4.42797 .000 4.347
10 min 93.1765 3.67823 81.8421 7.41068 .000 5.703
11 min 93.4667 5.08312 84.2500 3.33371 .000 5.409
12 min 94.5714 5.28700 83.0000 3.53553 .002 4.235
13 min 95.0000 2.82843 81.0000 - 0.09 7
73
TIME (MINUTES)
MEA
N B
LOO
D P
RES
SUR
E (m
mH
g)
BASELINE 1 2 3 4 5 6 7 8 9 10 11 12 13
60
80
100
120Group 1
Group 2
Graph No. 6: Comparison of MBP among two groups
Both the groups had similar preinduction MBP; however, after SAB the mean
Mean blood pressure was higher in the infusion group and was statistically significant.
74
INCIDENCE OF HYPOTENSION: The incidence of hypotension in group I, group II
was 3.57% and 100% respectively and the number of episodes of hypotension in group I
and group II were 2 and 54 episodes respectively as shown in Table 8 and Graph 9. It is
considered to be statistically significant with p value of .0001
Table No. 8: Comparison of incidence/episodes of hypotension between two groups
Incidence of Hypotension
Group I (n=25)
Group II (n=25)
Absent 24 (96.42) 25 (100%)
Present 1(3.57) 0
Episodes 2 54
Inference Number of episodes of Hypotension is significantly less in Group I and significantly more in Group II with p=0.0001
In group I there were 2 episodes of hypotension in 1 patient who required 2
boluses of phenylephrine in addition to the infusion for the correction of hypotension. In
the group II all 25 patients had episodes of hypotension which required treatment with
bolus doses of phenylephrine.
75
Graph No. 7: Comparison of incidence of hypotension among two groups
Graph No. 8: Comparison episodes of hypotension among two groups
76
USAGE OF PHENYLEPHRINE: The mean dose of phenylephrine used
intraoperatively in group I, group II were 496 ±280.59 and 216 ±94.33 respectively and
was significantly higher in group I as shown in Table 9 and graph 9.
Table No. 9: Comparison of use of phenylephrine (µg) in two groups
Group I Group II P value t value
TOTAL PHENYLEPHRINE USED
496 ±280.59 216 ±94.33 .0001 4.73
B
PHY
NY
LEPH
RIN
E D
OSE
(mcg
)
GROUP 1 GROUP 20
200
400
600
800
1000
Graph No. 9: Comparison of use phenylephrine (µg) in two groups
77
INTRAVENOUS FLUIDS: The mean volume of fluid used intraoperatively in group I,
group II were 105.60 (SD14.74) ml, 104.00 (SD 12.24) respectively and showed no
significant difference between the two groups as shown in Table 10 and Graph 10.
Table No. 10: Comparison of intraoperative fluid use between two groups
Group I Group II P value
t value
TOTAL VOLUME OF RINGER LACTATE INFUSED
105.60±14.74 104.00±12.24 0.678 .417
F
TOTA
L V
OLU
ME
INFU
SED
(ml)
GROUP 1 GROUP 20
50
100
150
Graph No. 10: Comparison of intraoperative fluid use between two groups
78
DURATION FROM SKIN INCISION TO DELIVERY OF BABY
The mean duration from skin incision to delivery of baby, in group I, group II
were 532.8±60.17 sec, 530.4±59.19 sec respectively and showed no significant difference
between the two groups
Table No. 11: Comparision of duration from skin incision to delivery of baby
Group I Group II P value t value
DURATION FROM SKIN INCISSION TO DELIVERY OF BABY
532.8 ± 60.17
530.4 ± 59.19
0.89 0.142
TIM
E (S
EC
ON
DS)
GROUP 1 GROUP 20
200
400
600
800
Graph No. 11: Comparision of duration from skin incision to delivery of baby
79
COMPLICATIONS: There were no incidences of complications such as nausea and
vomiting after induction of SAB
UMBILICAL ARTERY BLOOD pH: The mean value of Umbilical artery blood pH in
group I and Group II were 7.1736±0.03121 and 7.1756±.02740 respectively and showed
no significant difference between the two groups.
Table No. 12: Comparison of umbilical artery blood pH
Group I Group II P value t value
Umbilical artery blood pH
7.17±0.03 7.17±0.02 0.811 -0.241
R
UM
BILI
CA
L A
RTE
RY
BLO
OD
pH
GROUP 1 GROUP 27.0
7.1
7.2
7.3
7.4
Graph No. 12: Comparision of umbilical artery blood pH
80
APGAR SCORE:
The mean value of APGAR score at 1 min in group I and Group II were
8.84±0.80 and 9.12±0.66 respectively and showed no significant difference between the
two groups
The mean value of APGAR score at 1 min in group I and Group II were
9.68±0.47 and 9.80±0.40 respectively and showed no significant difference between the
two groups
Table No. 13: Comparison of APGAR scores between two groups
APGAR score Group I Group II P value t value
1 minute 8.84±0.80 9.12±0.66 0.185 -1.345
5 minute 9.68±0.47 9.80±0.40 0.344 -.957
V
APG
AR S
CO
RE
GROUP 1 GROUP 25
6
7
8
9
10
Graph No. 13: Comparison of APGAR Scores between two groups at 1 minute
81
V
APG
AR S
CO
RE
GROUP 1 GROUP 25
6
7
8
9
10
11
12
Graph No. 14: Comparison of APGAR scores between two groups at 5 minutes
82
DISCUSSION
Following spinal anaesthesia for Caesarean section hypotension remains a major
drawback with an incidence reported in the literature of upto 85%. This is inspite of
pregnant patients having 40-50% of more blood volume at term compared to nonpregnant
patients. Pregnant patients at term are more prone to develop hypotension due to the
occurrence of aortocaval compression by the foetal head and higher level of sympathetic
blockade owing to increased spread of local anaesthetic in the cerebrospinal fluid.
Hypotension, hazardous to the mother and more so, to the foetus, is better prevented than
treated. Blood pressure is usually maintained in the face of vasodilation, caused due to
factors other than central neural blockade, by a reflexive increase in cardiac output.
However, in the presence of spinal induced venodilation, venous return is reduced to an
extent that cardiac output cannot increase and is often reduced. The result is severe
hypotension with reduced uteroplacental perfusion and APGAR score.
Hypotension has been variously defined as reduction in pressure of 30 mm Hg, a
reduction to less than 100 mm Hg or as a reduction in arterial pressure of 20% below
baseline pressure. It has been shown that the percentage decrease in placental perfusion is
related to the percentage reduction in maternal arterial pressure and not to the absolute
reduction in pressure. For the purposes of this study, hypotension was defined as a
decrease in arterial pressure greater than 20 % from baseline systolic pressure. 31
Most strategies for decreasing the incidence of hypotension during spinal
anaesthesia for cesarean delivery have not proved to be reliable. Although early work
suggested that intravenous prehydration with crystalloid solutions was effective, this has
been questioned in more recent articles. Use of colloid solutions may be more effective
83
than crystalloids but the benefits are still limited, and infusion of large volumes of colloid
may have other risks, including fluid overload, interference with coagulation and
anaphylactoid reactions. Compression of the lower limbs has been described as an
alternative technique but is not convenient and is not popular. Traditionally ephedrine has
been recommended in this role. A number of other studies have recently reported on the
use of α agonists in obstetrics.46
Pure -agonist vasopressors initially were considered contraindicated in
obstetrics, because early experimental studies reported a substantial decrease in
uteroplacental blood flow linked to their vasoconstrictive properties. However, doses
used in these studies were much higher than those needed clinically in humans, although
they were appropriate to the species studied to restore spinal anaesthesia–induced
hypotension. In addition, a more recent experimental study suggested that pregnancy is
associated with an attenuated uterine vascular response to phenylephrine. Clinical studies
in women undergoing scheduled cesarean delivery have confirmed that small (40–100µg)
bolus doses of phenylephrine used to counteract hypotension during epidural or spinal
anaesthesia were effective and as safe as ephedrine bolus doses for the mother and the
neonate. 34
Our current study aims at comparing prophylactic infusion of phenylephrine and a
control group not receiving the infusion to prevent hypotension during spinal anaesthesia
for cesarean section. But both the groups received a bolus dose of phenylephrine 100µg
intravenous to treat any episodes of hypotension.
In our study, there were 50 patients of similar age group of 20-35yrs undergoing
elective cesarean section. They were randomly allotted into 2 groups of 25 each. In
84
Group I patients received intravenous prophylactic phenylephrine infusion immediately
after completion of intrathecal injection of Bupivacaine whereas the group II did not
receive the infusion. intravenous phenylephrine bolus 100µg was given when SAP is
decreased to <80% of baseline in both the groups. Following which the parameters were
studied.
In our study, there was no significant difference in the demographic parameters,
so the results of other parameters were comparable. There was no significant difference
in the level of blockade and intravenous fluid preloading between the groups.
Effect on maternal hemodynamics:
Heart rate: Here we observed that during the initial part of the study at 1 to 2 minute and
later part of the study from 10th to 11th minute the heart rate was higher in the group II
patients compared to that of group I. This is probably due to reflex bradycardia caused by
the phenylephrine infusion in group I which lowered the heart rate. But between the 3rd
and 9th minute the heart rate was comparable in both the groups. This was because of the
phenylephrine boluses given to the patients in group II to treat the hypotension episodes
which caused reflex bradycardia. But none of the patients require treatment with atropine
in both the groups. The above findings suggests infusion keeps the heart rate uniformly
but on a lower side compared to the boluses where a fluctuation in the hear rate was
observed.
Sharma and colleagues 41 found that the mean heart rate decreased significantly
after administration of phenylephrine boluses whereas it remained high in the patients
receiving mephentermine. Also Thomas and colleagues 32found that more than 50% of
women given phenylephrine developed significant bradycardia compared to the
85
ephedrine group. As cardiac output is the product of heart rate and stroke volume, this
suggests that phenylephrine restored a greater stroke volume than ephedrine. Because
phenylephrine (but not ephedrine) is virtually devoid of β inotropic effect, the better
stroke volume produced by phenylephrine probably reflects a much better preload than
with ephedrine, i.e., a better control of venous pooling caused by venoconstriction. But in
ephedrine group cardiac sympathetic denervation was masked by the chronotropic effect
of this β adrenergic agonist. Hall and colleagues31 also recorded 2 cases of bradycardia in
pheneylephrine group which was less than 40beats/min which was corrected with a bolus
dose of atropine and both these episodes occurred after multiple doses of phenylephrine .
No other patient had developed bradycardia. These finding were consistent with our
study and suggests that phenylephrine causes reflex bradycardia.
Blood pressure: In our study, we also observed that the incidence of hypotension is
3.57% (n=1/25) in group I and 100% in group II. It was observed that the incidence of
hypotension was higher in group II. This reflects a more stable management of blood
pressure can be achieved by phenylephrine infusion as it uniformly maintains the plasma
level of this vasopressor.
In our study we observed that the difference in systolic blood pressure, diastolic
blood pressure and mean blood pressure were highly significant between the two
groups.
The SBP, DBP and MBP were consistently higher in the infusion group when
compared to the control group. This probably was due to the stimulation of post synaptic
α receptors by phenylephrine resulting in intense arterial and peripheral venoconstriction
causing rise in blood pressure.
86
However, we found that the required dose of phenylephrine was much higher in
the infusion group than the control group. At term, uterine vascular bed is maximally
vasodilated and unable to autoregulate when perfusion pressure is reduced. Consequently
a higher adrenoceptor density renders uteroplacental blood flow potentially vulnerable to
vasoconstriction induced by α adrenergic agonists. Indeed infusion of phenyylephrine @
8µg/kg/min has been reported to decrease ovine uteroplacental blood flow by 50%
however the relationship between phenylephgrine dose and uterine vascular resistance is
not linear and dramatic increases in Uterine vascular resistance seen only to appear with
doses greater than 100µg/min thus, the satisfactory fetal outcome in human studies may
simply reflect the lower doses used. This which is consistent with our study where the
infusion rate was 100µg/min. 32
Non hemodynamic side effects:
In our study group none of the patients who received phenylephrine had nausea or
vomiting.
Cooper and colleagues37 suggest that that the possible explanation for nausea and
vomiting is an increase in vagal tone following reduction of preload. Cardiac preload
decreased in spinal anaesthesia, but phenylephrine a pure α- agonist, provides better
venoconstriction, reducing the decrease in cardiac preload and diminishing the vagal
reflex.
Sarvanan and collegues40 found that among the patients with ineffective blood
pressure control, phenylephrine was significantly better compared to ephedrine in the
prevention of vomiting.
87
All the above mentioned studies demonstrated lower incidence of nausea and
vomiting in patients receiving phenylephrine which is in accordance with our study.
Neonatal outcome:
The APGAR scores and measured umbilical artery blood pH were used to
indicate adequacy of placental perfusion. Despite periods of maternal hypotension in
group II and decreased heart rate in group I, we found no significant difference in either
APGAR score or UAB pH between 2 groups. This could be due to immediate correction
of hypotension episodes and thus maintenance of uteroplacental perfusion in both the
groups.
The APGAR score were similar in the groups and never less than 8, although the
incidence of arterial pH <7.18 was greater than desired. However this is not new
information. Several studies have reported a surprisingly high incidence of acidosis (not
accompanied with neonatal depression) after spinal anaesthesia for cesarean deliveries. 34.
Another mechanism for decreased uterine artery blood pH is by prolonged period of
decreased maternal cardiac output occurring before delivery. Robson and colleagues
found that UAB pH correlated well with maternal cardiac output (but not with BP
itself).29
Also, Hall and coworkers found that despite periods of maternal hypotension,
which occurred longer than 2 min, and periods of maternal bradycardia, there was no
significant difference in either APGAR scores or blood-gas data between three groups.31
It was also shown by Joupilla and colleagues that intravenous preload maintains
placental blood flow despite moderate reduction in maternal pressure, thus minimizing
fetal acidosis. In our study we had taken precautions by preloading the patients with
88
10ml/kg of Ringer lactate solution which probably would have maintained placental
blood flow during hypotensive episodes lasting longer than 2 minutes.26
Previous studies have also shown that phenylephrine either in the form of bolus or
infusion has no neonatal adverse effects28, 43, 45
In our study, the observed decrease in UAB pH without a reduction in APGAR
scores may be due to reduced CO during delivery and the maintenance of uterine
perfusion by adequate preload.
Advantages and limitations of our study: Our study design had an inherent advantage
that only phenylephrine was used for all the patients and no other drug was given
intraoperatively before extraction of the baby. This makes the possibility of influences of
other drugs on our study drug remote. In our study group all the patients had similar
demographic parameters which made their influence very unlikely. However there were
some pitfalls also. Patient factors like psychological makeup might have had a bearing
effect on our observation. The tissue traumas related to the extent of surgery too have had
contributory effect. Finally small sample size in each group might have limited the true
clinical significance of our comparison.
89
CONCLUSION
The prophylactic administration of intravenous phenylephrine in ASA II patients
undergoing elective cesarean surgery under spinal anaesthesia is an effective measure in
preventing hypotension without causing untoward side effects like central nervous system
stimulation, tachycardia or arrhythmias in the mother and neonates.
In conclusion, these data suggest that a prophylactic phenylephrine infusion is an
effective and simple method of reducing the incidence of hypotension during spinal
anaesthesia for cesarean delivery, with no adverse effect on neonatal outcome.
90
SUMMARY
This prospective randomized comparative study was designed to know the
efficacy and safety of prophylactic phenylephrine in prevention of spinal anaesthesia
induced hypotension.
The study was carried on singleton full term pregnant patients, age 20- 35yrs of
ASA grade II scheduled for elective cesarean section under spinal anaesthesia in A.J.
Institute of Medical Sciences. They were randomly allocated into two groups of 25 each.
Group I- The patient received intravenous prophylactic phenylephrine infusion at
100µg/min for 3min after completion of intrathecal injection. Then each min SAP is
measured and infusion stopped if SAP> baseline and will be continued or restarted if less
than or equal to baseline SAP. Intravenous phenylephrine bolus 100µg was given when
SAP is decreased to <80% of baseline.
Group II - The patients received intravenous phenylephrine bolus 100µg when
SAP is decreased to <80% of baseline
After premedication Baseline SAP, DAP and HR was noted. On receiving the
patient to OT, monitors were connected and vital signs were recorded. Patients were
preloaded with 10ml/kg of ringer’s lactate over 15 minutes. Then intravenous lactated
Ringer’s solution was started at 10 mL/min.
Spinal anaesthesia was induced with patients in the lateral position with a 23-
gauge Quinche babcocks needle at the L2-3 or L3-4 vertebral interspace, and hyperbaric
0.5% bupivacaine 2.0 mL was injected intrathecally. Patients were then immediately
turned supine with left uterine displacement with help of a wedge. SAP was measured at
1-min intervals beginning 1 min after spinal injection.
91
Immediately after the completion of intrathecal injection, phenylephrine infusion
was started in the group I patients at 1 mL/min (100 µg/min), whereas patients in the
group II did not have it. Infusion was continued for a minimum of 3 min, after which the
infusion was either stopped or continued according to a predefined protocol based on the
SAP measurement each minute. After each 1-min measurement of SAP, the infusion was
stopped if the SAP was more than baseline, and it was continued or restarted if the SAP
was less than or equal to baseline. For the purposes of the study, we defined hypotension
as a decrease in SAP to <80% of baseline. Each time there was a SAP measurement
showing hypotension, patients received a 100 µg intravenous bolus of phenylephrine both
in group I and group II.
Oxygen was routinely given at 4 L/min by clear face mask. Any incidences of
nausea (reported by patients) or vomiting (observed by investigators) were recorded. We
planned to treat nausea or vomiting that was not associated with hypotension with
intravenous ondansetron 8mg and to treat bradycardia, defined by an HR <50 bpm with
intravenous atropine 0.6mg.
After intrathecal injection, the upper sensory level of anaesthesia was measured
by assessing loss of pinprick discrimination. Further checks of the block height were
made as required before the start of surgery, but these levels were not recorded as part of
the study. The times of skin incision, uterine incision, and delivery were recorded. After 1
minute of SAB; HR, SAP and DBP were recorded every minute till the extraction of the
baby. The infusion and bolus protocol was continued until the time of delivery of the
baby, after which further management was at the discretion of the attending
anesthesiologist, who was free to administer intravenous fluids and vasopressors as
92
appropriate to replace surgical losses and maintain SAP. The total volumes of study
solutions given up to the time of delivery of the baby were recorded.
After delivery, oxytocin 20 IU in 1000 ml saline was given by slow intravenous
infusion. APGAR scores were assessed 1 and 5 min after delivery. Umbilical artery blood
samples were taken from a double-clamped segment of umbilical cord by for immediate
blood gas analysis.
These observations were analyzed to get information on incidence of hypotension,
the effect of the prophylactic phenylephrine on the maternal hemodynamics and its
consequences, effect of the prophylactic phenylephrine on the APGAR scores, umblical
artery blood pH and intraoperative requirements of phenylephrine.
It was observed that infusion keeps the heart rate uniformly but on a lower side
compared to the boluses where a fluctuation in hear rate was observed. But none of
the patient required treatment with intravenous atropine.
The incidence of hypotension is 3.57% (n=1/25) in group I and 100% in group II. It
was observed that incidence of hypotension is higher in group II.
The SBP, DBP and MBP were consistently higher in the group I when compared to
the group II.
We found that the dose of Phenylephrine was much higher in the infusion group than
the control group which was statistically significant (p value =0.0001)
In our study group none of the patients had any incidence of nausea or vomiting.
It was observed that there was a decrease in UAB pH without a reduction in APGAR
scores which may be due to reduced CO during delivery and the maintenance of
uterine perfusion by adequate preload. There was no significant difference between
the two groups in either the APGAR scores or UAB pH. (p>0.05)
93
BIBLIOGRAPHY
1. Hughes SC, Levinson G, Rosen MA. Anaesthesia for Caesarean section, In:
Anaesthesia for Obstetrics, 4th ed, Philadelphia Lippincott, Williams and Wilkins
1993: pp 201-36.
2. Rout C.C and Rocke D.A. Prevention of Hypotension Following Spinal Anaesthesia
for Cesarean Section. International Anesthesiology Clinics. 1994; 32:117-135.
3. Birnbach DJ and Browne IM. Anesthesia for obstetrics. In: Miller DR Edt. Miller’s
Anaesthesia. 7th ed. Philadelphia: Elsevier Churchill Livingstone. 2010; 2203-40
4. Bridenbough. P. O, Greene. N. M, Brull. J. S, Spinal (subarachnoid) Neural blockade.
In: Cousins. M. J and Bidenbaugh. P.O Edt: Neural blockade in clinical Anaesthesia
and management of pain, 3rd ed. Philadelphia, Lippincott- Raven publisher, 1998;
203-241.
5. Colin .P. Spinal anaesthesia- principles In: Principles of Anesthesiology general and
regional anaesthesia. 3rd ed. Philadelphia, 1993; volume 2, 1445-1497.
6. Mcleod G. Spinal analgesia: Intradural and extradural. In: Davies NJH, Cashman JN
Edt. Lee’s synopsis of anaesthesia. 13th ed. Noida: Butterworth Heinemann. 2006;
471-536.
7. Kleinman W. Spinal, epidural and caudal blocks. In: Morgan EG, Mikhail SM and
Murray JM Edt. Clinical anesthesiology. 3rd ed. New Delhi: Lange Medical Books,
McGraw Hill Medical Publishing Division. 2002; 253-282.
94
8. Chaurasia BD, ed. Bones and joints of thorax. In: Human anatomy, Regional and
clinical applied dissection. 4th ed. New Delhi: CBS Publishers and Distributors.
2004; 189-204.
9. Ellish H, Feldman S and Griffiths OHW, edt. The vertebral canal and its contents. In:
Anatomy for Anaesthetists. 8th ed .Oxford: Blackwell Publishing. 2004; Part 3;
95-135
10. Greene.N. M, Brull. S. J, Gillies. J, The cardiovascular system. In: Greene N.M. and
Brull S.J Edt. Physiology of Spinal Anaesthesia. 4th ed. Baltimore: Williams and
Wilkins, 1993:85-199.
11. Lee. J. A, Atkinson. R. S, Watt. M. J. edt: Physiology of central neural blockade. In:
Atkinson and Lee- Sir Robert Macintosh’s Lumbar Puncture and Spinal Analgesia
Intradural and extradural. 5th edition. New York: Churchill Livingstone, 1985:98-117.
12. McCrae A.F, Wildsmith J.A.W. Prevention and Treatment of Hypotension during
Central Neural Block. British J. Anaesth. 1993; 70:672-680.
13. Liu S.S, McDonald S.B. Current Issues in Spinal Anaesthesia.Anesthesiology.2001;
94:5:888-907.
14. Critchley L.A.H. Hypotension, Subarachnoid block and the elderly patient.
Anaesthesia. 1996; 51, 1139-1143.
15. Wong CA, Norris MC. Acute situations: Obstetrics, Chapter 25, Textbook of
Regional Anaesthesia, Prithvi Raj P, Churchill Livingstone 2002: pp 471-494.
16. Wright RG, Shnider SM. Hypotension and regional anaesthesia on Obstetrics,
Chapter 22, Anaesthesia for Obstetrics, 3rd ed, Williams and Wilkins 1993:
pp 397-404.
95
17. Sadhu G. Prevention of hypotension during regional anaesthesia for caesarean
section - Effective use of vasopressors. Specialist Library for Surgery, Theatres and
Anaesthesia, National Library for Health [published August 2008]
18. Margaret W. Local anesthetic agents. In: Wood M and Wood JJA Edt. Drugs and
anaesthesia. Pharmacology for Anaesthesiologist. 2nd ed, London: Williams and
Wilkins. 319-345.
19. Morgan. E. G, Mikhail. S. M, Murray JM edt: Local Anaesthetics. in: Clinical
Anesthesiology. 3rd Ed. New Delhi: Lange Medical Book. McGraw Hill Medical
Publishing Division. 2002:233-241.
20. Stoelting RK. Local anesthetics. In: Robert KS. Robert KS Ed. Pharmacology and
physiology in anesthetic practice. 4th ed. Philadelphia: Lippincott Williams and
Wilkins 2006; 179-207.
21. Strichartz. G. R, Berde. C. B. Local Anesthetics. In: Miller DR Edt. Miller’s
Anaesthesia. 7th ed. Philadelphia: Elsevier Churchill Livingstone. 2010;913-40.
22. Dollery C, ed. phenylephrine (hydrochloride). In: Therapeutic drug. 2nd ed. Edinburgh
(UK) : Churchill Livingstone.1999; 104-7.
23. Sweetman SC, ed. Cough suppressants, Expectorants, mucolytics and nasal
decongestants. In: Martindale The complete drug reference.34th ed. London:
Pharmaceutical Press Publishers. 2005; 1126-27.
24. www.wikipedia.org/wiki/phenylephrine on 12th June 2011.
25. www.apps.aahs.org/criticalcare/phenylephrine%20(neosynephrine).pdf on 10th
December 2011.
96
26. Jouppila P, Jouppila R, Barinoll T, Koivula A. Placental blood flow during Caesarean
section performed under subarachnoid blockade. Br J Anaesth 1984;56: 1379.
27. Bhagwanjee S, Rocke DA, Rout CC, et al. Prevention of hypotension following
spinal anaesthesia for elective caesarean section by wrapping of the legs. Br J
Anaesth 1990; 65:819–22.
28. Moran DH, Perilo M, La Porta RF, Bader AM, Datta S. phenylephrine in the
prevention of hypotension following spinal anaesthesia for Cesaerean delivery. J Clin
Anesth 1991; 3: 301–5.
29. Robson SC, Boys RJ, Rodeck C, Morgan B: Maternal and fetal haemodynamic
effects of spinal and extradural anaesthesia for elective caesarean section. Br J
Anaesth 1992; 68:54–9.
30. Rout CC., Rocke DA. and Gouws E: Leg elevation and wrapping in the prevention of
hypotension following spinal anaesthesia for elective Caesarean section. Anaesthesia,
1993; 48: 304–308.
31. Hall PA, Bennett A, Wilkes MP, Lewis M. Spinal anaesthesia for Caesarean section:
comparison of infusions of phenylephrine and ephedrine. Br J Anaesth 1994; 73:
471–4.
32. Thomas DG, Robson SC, Redfern N, Hughes D, Boys RJ. Randomised trial of bolus
phenylephrine or ephedrine for maintenance of arterial pressure during spinal
anaesthesia for Caesarean section. Br J Anaesth 1996; 76: 61–5.
33. Nagan kee WD, Khaw KS, Lee BB, Ng FF and Wong MMS. Randomized controlled
study of colloid preload before spinal anaesthesia for Caesarean section. Br J Anaesth
2001; 87: 772–4.
97
34. Mercier JF, Riley ET, Fredericson WL, Roger-Christoph S, Benhamou D, Cohen SE.
Phenylephrine added to prophylactic ephedrine infusion during spinal anesthesia for
elective Cesarean section. Anesthesiology 2001; 95: 668–74.
35. Ayorinde BT, Buczkowski P, Brown J, Shaw J, Buggy DJ. Evaluation of preemptive
intramuscular phenylephrine and ephedrine for reduction of spinal anaesthesia
induced hypotension during Caesarean section. Br J Anaesth 2001; 86: 372–6.
36. Ngan Kee WD, Lau TK, Khaw KS, Lee BB. Comparison of metaraminol and
ephedrine infusions for maintaining arterial pressure during spinal anesthesia for
Cesarean section. Anesthesiology 2001; 95: 307–13.
37. Cooper DW, Carpenter M, Mowbray P, Desira WR, Ryall DM, Kokri MS. Fetal and
maternal effects of phenylephrine and ephedrine during spinal anesthesia for
Cesarean delivery. Anesthesiology 2002; 97: 1582–90.
38. Loughrey JPR, Yao N, Datta S, Segal S, Pian-Smith M, Tsen LC. - Hemodynamic
effects of spinal anesthesia and simultaneous intravenous bolus of combined
phenylephrine and ephedrine versus ephedrine for cesarean delivery. Int J Obstet
Anesth, 2005; 14:43-47.
39. Ngan Kee WD, Khaw KS, Ng FF: Prevention of hypotension during spinal anesthesia
for cesarean delivery: An effective technique using combination phenylephrine
infusion and crystalloid cohydration. Anesthesiology, 2005; 103: 744–50.
40. Saravanan S, Kocarev M, Wilson RC, Watkins E, Columb MO, Lyons G: Equivalent
dose of ephedrine and phenylephrine in the prevention of post-spinal hypotension in
Caesarean section. Br J Anaesth, 2006; 96:95-99.
98
41. Sharma R, Maitra N and Niyogi M: A Comparative Study of Bolus phenylephrine
and mephentermine for Treatment of Hypotension during Spinal Anesthesia for
Cesarean Section. The Internet Journal of Anesthesiology. 2009 Volume 19
Number 2.
42. Ngan Kee WD, Lee A, Khaw KS, Ng F, Karmakar MK, Gin T. A Randomized
Double-Blinded Comparison of phenylephrine and ephedrine Infusion Combinations
to maintain blood pressure during spinal anesthesia for cesarean delivery: The effects
on fetal acid-base status and hemodynamic control. Anesth Analg 2008;107:1295-
1302.
43. Prakash S, Pramanik V, Chellani H, Salhan S, Gogia AR. - Maternal and neonatal
effects of bolus administration of ephedrine and phenylephrine during spinal
anaesthesia for caesarean delivery: a randomized study. Int J Obstet Anesth,
2010;19:24-30.
44. Dyer RA, Reed AR, van Dyk D, Michelle J. Arcache, Hodges O, Lombard CJ,
Greenwood J, James MF. Hemodynamic effects of ephedrine, phenylephrine, and the
coadministration of phenylephrine with oxytocin during spinal anesthesia for elective
cesarean delivery. Anesthesiology, 2009; 111:753-765.
45. Ngan Kee WD, Khaw KS, Tan PE, Ng FFRN, Karmakar MK. - Placental transfer and
fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for
cesarean delivery. Anesthesiology, 2009; 111:506-512.
46. Pinto V., Jaysundara N., Abeysundara A., Ekanayake S. Use of phenylephrine as
vasopressor of choice to prevent hypotension following spinal anaesthesia in LSCS.
SL J Anaesth 2009; 16(2) : 74 - 78
99
ANNEXURE
PROFORMA
A) NAME:
B) AGE:
C) SEX:
D) IP NO:
E) DIAGNOSIS:
F) ASA GRADE:
G) PRIMI, SINGELTON:
H) HEIGHT:
I) WEIGHT:
J) GESTATIONAL AGE:
K) PREMEDICATION GIVEN:
L) PLAN OF ANAESTHESIA:
1) TABLE 1: PRE OP VITALS
HR SBP DBP MBP TEMP
2) FHS ASSESSMENT ( PREOP)
3) PRELOADING
100
4) SPINAL ANAESTHESIA DRUG INJECTED AT:
PHENYLEPHREINE INFUSION STARTED AT:
5) TABLE 2: SPINAL ANAESTHESIA
Nee
dle
size
Dos
e m
g
Dru
g
Vol
in m
l
Wed
ge
Lt ti
lt
Hea
d up
Leve
l of b
lock
Ons
et
Dur
atio
n
Blo
od ta
p/
tinge
6) TABLE 3: VITALS READINGS
BASE LINE: HEART RATE-
SBP-
DBP-
MBP-
Tim
e (m
in)
Dos
e of
ph
enyl
ephr
ine
HR
SBP
DB
P
MB
P
Add
ition
al
vaso
pres
sor
Atro
pine
Vol
ume
infu
sed
Oxy
toci
n
101
7) EFFICACY OF BLOCK
LATENCY:
ADEQUACY OF BLOCK
EXCELLENT:
ADEQUATE:
POOR- SEDATION NEEDED:
CONVERTED TO GA:
OXYGEN GIVEN OR NOT
8) DOSE OF METHERGINE:
DOSE OF PROSTADINE:
9) INDUCTION- DELIVERY TIME:
SKIN INCISSION- DELIVERY TIME:
UTERINE INCISSION- BABY EXTRACTION TIME:
10) NEONATAL FACTORS
BABY CRIED IMMEDIATELY AFTER BIRTH- YES/ NO
APGAR SCORE: at 1 minute
at 5 minute
UMBILICAL ARTERY BLOOD pH :
102
CONSENT FORM
FOR OPERATION/ANAESTHESIA
I ___________________ Hosp. No.____________ in my full senses hereby give my
complete consent for ________________ or any other procedure deemed fit which is a
therapeutic / and diagnostic procedure / biopsy / transfusion / operation to be performed
on me / my son / my daughter / my ward __________ age __________ under any
anaesthesia deemed fit. The nature and risks involved in the procedure have been
explained to me to my satisfaction. For academic and scientific purpose the
operation/procedure may be televised or photographed.
Date: Signature/Thumb Impression of Patient/Guardian
Name: Designation:
Guardian:
Relationship:
Full Address:
103
KEY TO MASTER CHART APG SC 1 → APGAR score at 1 minute
APG SC 5 → APGAR score at 5 minute
DBP → Diastolic Blood pressure in mm Hg
BDBP → Baseline Diastolic Blood pressure in mm Hg
BHR → Baseline heart rate in beats per minute
BMBP → Baseline mean blood pressure in mm Hg
BSBP → Baseline systolic blood pressure in mm Hg
Group I → Phenylephrine Infusion
Group II → No phenylephrine Infusion
HR → Heart rate in beats per minute
HT → Height in centimeters
I. P. No. → Inpatient Number
PHE → Phenylephrine
POG → Period of gestation
PT → Patient
MBP → Mean blood pressure in mm Hg
NO → Number
SBP → Systolic blood pressure in mm Hg
TVI → Total volume infused
UAB pH → Uterine artery blood pH
SID → Skin incision to baby delivery time in seconds
WT → Weight in Kilograms
SBP → Blood Pressure in mm Hg
Yrs → Years
104
Master chart Group I
PT N
O
PT N
AM
E
PT IP
NO
PT A
GE
(Yrs
)
PTW
T
PT H
T
POG
BH
R
BSB
P
BD
BP
BM
BP
HR
-1ss
t min
HR
– 2
nd m
in
HR
– 3
rd m
in
HR
– 4
th m
in
HR
– 5
th m
in
HR
– 6
th m
in
HR
– 7
th m
in
HR
– 8
th m
in
HR
– 9
th m
in
HR
– 1
0th m
in
HR
– 1
1th m
in
HR
– 1
2th m
in
HR
– 1
3th m
in
1 Annapoorna 584920 22 64 153 39W 2 D 94 114 76 89 98 96 95 90 88 86 88 89 90 86 85 2 Mookambika 648056 29 69 160 39W 99 131 84 100 96 92 100 96 98 99 100 90 92 91 88 3 Farida 624596 25 65 156 39W1D 88 122 71 88 86 88 84 82 84 86 87 88 90 4 Beebi 487537 23 64 152 39W2D 88 118 70 86 86 90 92 90 88 88 90 86 82 86 90 88 5 Surekha 332595 28 58 158 38W4D 93 120 76 91 101 92 97 74 76 78 78 80 90 6 Jayalaxmi 690176 30 60 155 37W5D 80 127 69 88 82 86 88 87 85 89 85 84 90 88 86 7 Thara 529693 24 68 154 39W1D 90 122 68 86 88 86 90 92 91 89 90 89 8 Manjula 696487 20 60 156 38W2D 88 124 76 92 90 92 88 90 88 90 91 93 95 9 Malini 695362 30 70 156 38W2D 91 128 79 95 97 98 95 92 90 88 90 92 95 93
10 Navya 695514 25 60 150 39W 83 126 78 94 88 85 87 86 87 90 88 91 87 89 90 11 Bhavya 696134 26 70 168 39W1D 92 119 78 92 83 92 80 76 80 74 72 70 68 76 12 Usha 345331 20 75 168 39W3D 92 124 81 95 98 95 94 95 92 93 95 91 90 89 90 92 93 13 Ramya 461655 26 55 160 38W 103 124 76 92 100 96 90 86 82 80 92 96 88 92 96 90 14 Sandhya 674224 30 60 166 39W 104 106 66 79 108 106 100 98 96 95 97 99 100 95 94 93 15 Bhagya 680292 28 68 162 39W5D 89 120 75 90 80 77 95 88 97 96 88 86 90 92 96 98 16 Fouziya 106914 30 66 156 38W5D 74 141 80 100 76 74 72 78 77 69 80 80 86 78 76 17 Rathna 701684 23 80 156 38W2D 104 134 70 91 76 72 76 80 82 76 74 72 68 62 78 18 Vanitha 698103 27 64 166 40W1D 98 128 80 96 84 100 98 108 94 92 88 86 68 92 84 99 98 19 Amitha 653164 24 62 156 37W5D 92 132 76 95 90 94 93 91 90 92 96 94 92 93 90 91 20 Sairabanu 580718 26 58 155 38W3D 92 135 75 95 90 88 87 90 92 88 90 91 92 90 89 21 Nmamatha 599234 25 61 156 40W3D 86 132 76 95 89 90 96 94 90 88 89 94 95 22 Ashalatha 610682 27 63 158 38W4D 85 124 74 91 86 88 90 86 88 82 90 84 88 88 85 23 Mamtaz 661876 25 60 156 40W4D 87 109 68 82 88 90 91 90 89 85 88 90 89 24 Harinakshi 597753 26 62 154 39W3D 86 110 69 83 86 88 90 89 91 93 89 90 83 25 Prathima 594411 27 63 156 38W2D 88 114 72 86 88 89 93 92 90 88 89 86 87
min
105
SBP
– 1ss
t min
SBP
– 2nd
min
SBP
– 3rd
min
SBP
– 4th
min
SBP
– 5th
min
SBP
– 6th
min
SBP
– 7th
min
SBP
– 8th
min
SBP
– 9th
min
SBP
– 10
th m
in
SBP
– 11
th m
in
SBP
-12th
min
SBP
– 13
th m
in
DB
P –
1st min
DB
P- 2
nd m
in
DB
P –
3dr m
in
DB
P –
4th m
in
DB
P –
5th m
in
DB
P -6
th m
in
DB
P –
7th m
in
DB
P –
8th m
in
DB
P –
9th m
in
DB
P -1
0th m
in
DB
P –
11th m
in
DB
P –
12th m
in
DB
P –
13th m
in
117 116 121 122 120 117 120 118 114 121 118 77 76 74 71 70 75 74 72 68 70 72
136 143 132 134 140 132 140 136 136 134 132 80 83 80 82 88 78 85 80 77 70 80
127 126 125 128 130 123 124 123 128 71 68 70 67 70 72 75 70 68
128 130 128 126 128 120 124 130 126 126 128 128 68 71 68 70 73 70 68 66 71 72 70 68
115 98 113 116 92 88 96 98 98 60 56 69 42 46 46 50 55 52
130 127 132 136 131 132 130 131 *128 136 133 71 68 72 77 70 72 70 73 70 76 70
121 124 129 122 121 128 129 126 70 73 68 74 70 76 75 74
135 130 131 128 131 122 133 136 130 80 78 83 80 78 69 72 80 82
130 125 128 135 130 128 129 136 126 125 83 72 76 71 74 80 70 69 70 76
131 130 127 132 136 129 134 130 129 136 133 80 83 78 81 86 75 72 78 71 78 77
115 118 114 117 122 106 108 120 100 127 75 72 76 80 75 70 70 65 68 86
123 120 116 111 128 136 130 121 130 132 127 130 126 75 74 61 70 80 87 70 66 88 75 78 76 83
123 120 124 120 124 131 136 127 126 130 129 136 89 80 76 87 70 82 83 80 70 83 84 88
103 100 104 111 106 131 136 138 147 128 130 121 70 61 72 80 70 79 80 88 91 80 76 83
118 115 122 116 121 112 118 122 120 123 112 110 76 83 76 70 75 68 78 68 72 78 66 78
127 130 126 113 118 120 123 124 131 130 125 86 84 79 70 76 68 80 76 81 78 82
133 130 132 124 127 130 132 135 128 126 136 81 76 77 76 80 82 80 83 76 70 82
126 119 133 126 124 110 127 126 132 121 126 129 120 82 77 86 84 82 60 62 83 86 80 84 80 79
136 133 134 133 132 134 137 134 137 130 134 135 76 77 76 74 77 70 72 77 74 70 74 75
136 139 136 134 135 130 135 136 132 133 138 74 76 81 76 76 74 73 76 74 72 75
132 129 134 128 127 130 132 127 126 75 78 74 77 70 76 74 75 70
129 130 130 133 128 131 126 128 131 126 125 76 74 77 78 76 80 77 72 74 71 72
121 122 118 116 117 120 115 110 112 70 71 70 68 66 71 72 74 71
118 120 126 129 126 124 123 118 66 71 72 70 69 68 70 72
120 122 123 120 116 119 120 118 118 76 74 75 70 74 71 70 75 70
106
MB
P -1
st min
MB
P –
2ndm
in
MB
P –3
rd m
in
MB
P- 4
th m
in
MB
P -5
th m
in
MB
P -6
th m
in
MB
P -7
th m
in
MB
P -8
th m
in
MB
P -9
th m
in
MB
P -1
0th m
in
MB
P -1
1th m
in
MB
P -1
2th m
in
MB
P -1
3th m
in
TVI
UA
B p
H
APG
SC
1
APG
SC
5
PHE
USE
D
SID
TIM
E
90 89 90 88 87 89 89 87 83 87 87 110 7.19 9 10 500 540
99 103 97 99 105 96 103 99 97 91 97 110 7.18 10 10 500 570
90 87 88 87 90 89 91 88 88 90 7.18 9 9 300 480
88 91 88 89 91 87 87 87 89 90 89 88 120 7.18 9 10 300 600
78 70 84 67 61 60 65 69 67 90 7.1 9 9 1100 480
91 88 92 97 90 92 90 92 89 96 91 110 7.16 10 10 400 540
87 90 88 90 87 93 93 91 80 7.17 9 10 300 480
98 95 99 96 96 87 92 99 98 90 7.2 8 9 400 480
99 90 93 92 93 96 90 91 89 92 100 7.18 10 10 500 480
97 99 94 98 103 93 93 95 90 97 96 110 7.21 8 10 300 600
88 87 89 92 91 82 83 83 79 100 100 7.18 9 10 700 600
91 89 79 84 96 103 90 84 102 94 94 94 97 130 7.16 10 10 500 600
100 93 92 98 88 98 101 96 89 99 99 104 120 7.11 8 10 500 480
81 74 83 90 82 96 99 105 110 96 94 96 120 7.21 8 9 400 600
90 94 91 85 90 83 91 86 88 93 81 89 120 7.2 9 10 1200 570
100 99 95 84 90 85 94 92 98 95 96 110 7.18 8 9 300 600
98 94 95 92 96 98 97 100 93 89 100 110 7.2 8 9 900 480
97 91 102 98 96 77 84 97 101 94 98 96 93 130 7.1 9 10 1100 540
96 96 95 94 95 91 94 96 95 90 94 95 120 7.15 8 10 400 660
95 97 99 95 96 93 94 96 93 92 96 110 7.21 10 10 300 540
94 95 94 94 89 94 93 92 89 90 7.18 9 10 300 480
94 93 95 96 93 97 93 91 93 89 90 110 7.2 10 10 300 540
87 88 86 84 83 87 86 86 85 90 7.16 8 10 300 480
83 87 90 90 88 87 88 87 80 7.18 8 9 300 420
91 90 91 87 88 87 87 89 86 90 7.17 8 9 300 480
107
Group - II PT
NO
PT N
AM
E
PT IP
NO
PT A
GE
PTW
T
PT H
T
POG
BH
R
BSB
P
BD
BP
BM
BP
HR
-1ss
t min
HR
– 2
nd m
in
HR
– 3
rd m
in
HR
– 4
th m
in
HR
– 5
th m
in
HR
– 6
th m
in
HR
– 7
th m
in
HR
– 8
th m
in
HR
– 9
th m
in
HR
– 1
0th m
in
HR
– 1
1th m
in
HR
– 1
2th m
in
HR
– 1
3th m
in
1 Sujatha 591380 22 63 156 40W3D 90 128 71 90 92 91 89 92 93 91 89 90 91
2 Fouzana 93351 21 60 152 39W4D 94 135 76 96 96 95 93 95 94 93 90 92 94 93 91
3 Vani 184271 22 62 152 38W3D 94 132 70 91 98 97 91 93 91 90 93 95 94
4 Nasita 601383 25 66 158 40W6D 89 120 69 86 90 88 87 86 86 88 90 91 92
5 Kushala 580608 25 67 156 38W5D 88 126 70 89 90 92 88 86 90 92 93 91 95 92 93
6 Sheela 604341 28 64 154 39W3D 91 125 64 84 90 91 90 89 91 93 92 91 90 89 92
7 Sahana 604178 26 60 156 39W1D 92 132 71 91 99 98 95 90 88 89 90 92 91 93 95
8 Shaila 598813 24 64 158 38W3D 95 134 76 95 96 93 91 93 90 88 90 91 93 94
9 Vijayalaxmi 602859 23 67 159 39W4D 91 128 72 91 94 92 91 93 90 89 90 93 95 96 95 93
10 Roopa 187893 26 67 157 39W1D 96 125 71 89 95 99 92 90 92 95 90 96 95 92
11 Fouzia 575618 23 64 155 38W5D 94 126 72 90 96 93 91 90 89 90 93 92 90 93 95
12 Ramya 605946 24 66 154 39W2D 97 122 74 90 99 96 92 93 90 89 92 90 91 91
13 Geetha 610681 24 63 152 39W2D 92 122 65 84 90 95 92 91 89 89 91 95 92
14 Seema 606821 26 64 155 39W2D 92 115 70 85 88 89 82 83 80 80 84 83 85 83
15 Saritha 579545 25 67 157 41W 92 121 72 88 99 96 95 90 91 93 94 95 93 91
16 Dilshad 73115 26 62 150 40W5D 94 114 71 85 99 96 88 86 80 84 86 82 88 87 95 96
17 Shahida 592385 24 67 160 39W3D 86 124 74 91 90 91 88 95 94 90 88 90 91 95
18 Sudharani 627273 22 65 157 38W6D 90 126 74 91 91 88 90 95 90 88 95 93 92 98 96 95
19 Divya 191523 24 66 159 38W5D 96 113 71 85 98 100 91 95 88 90 92 99 95 97 93
20 Sunanda 630657 27 69 153 40W5D 86 121 72 88 89 87 90 86 84 88 90 91 93 98 96 95 95
21 Latha 633650 28 66 160 38W5D 92 124 76 92 108 110 106 100 112 100 98 102 106 112 100
22 Usha 609879 30 66 156 38W4D 92 132 85 101 84 83 90 92 88 86 87 76 70 88
23 Kavitha 584485 28 68 154 39W 103 127 80 96 99 106 102 92 102 102 88 90 24 Gayathri 613718 25 64 157 39W 95 108 67 81 98 93 91 95 89 91 95 94 93 25 Shoba 634439 28 65 155 38W2D 87 126 74 91 92 95 88 89 87 84 82 80 85 91
108
SBP
– 1ss
t min
SBP
– 2nd
min
SBP
– 3rd
min
SBP
– 4th
min
SBP
– 5th
min
SBP
– 6th
min
SBP
– 7th
min
SBP
– 8th
min
SBP
– 9th
min
SBP
– 10
th m
in
SBP
– 11
th m
in
SBP
-12th
min
SBP
– 13
th m
in
DB
P –
1st min
DB
P- 2
nd m
in
DB
P –
3dr m
in
DB
P –
4th m
in
DB
P –
5th m
in
DB
P -6
th m
in
DB
P –
7th m
in
DB
P –
8th m
in
DB
P –
9th m
in
DB
P -1
0th m
in
DB
P –
11th m
in
DB
P –
12th m
in
DB
P –
13th m
in
131 121 102 95 107 111 114 113 110 76 73 68 67 68 71 68 72 66
138 131 121 103 101 110 114 120 126 125 128 78 76 70 66 67 70 67 70 72 70 68
137 130 118 100 101 111 116 119 116 76 71 70 68 4 69 66 69 69
124 121 101 91 92 90 103 110 113 73 70 69 63 64 60 67 68 70
131 116 98 102 104 111 112 116 114 118 120 118 74 70 68 70 67 68 70 73 69 72 73 72
130 124 100 96 101 108 114 117 113 111 109 68 65 57 58 62 69 68 70 72 69 68
138 127 108 100 102 110 100 106 98 110 108 78 74 76 68 64 68 66 71 68 72 74
135 130 115 101 98 104 107 106 110 116 78 73 68 71 66 68 71 74 72 69
136 131 118 104 100 98 110 116 119 115 114 117 77 76 71 72 67 59 65 70 73 68 68 71
132 118 100 92 98 103 110 107 108 110 76 74 60 58 58 60 62 63 68 66
127 116 98 95 97 102 109 110 108 102 103 76 71 72 68 64 67 66 69 70 69 71
130 111 92 90 110 106 108 100 107 103 78 68 64 65 70 68 71 62 69 70
128 116 105 100 96 105 104 107 104 68 64 65 62 61 62 62 68 66
116 106 90 86 83 90 103 110 112 110 69 67 64 60 58 60 67 71 72 70
121 115 96 89 92 96 102 108 111 108 70 68 60 58 58 60 62 62 64 65
116 100 88 96 110 106 90 99 108 110 106 108 68 68 61 58 68 68 60 65 69 68 68 70
131 128 101 92 98 106 120 106 108 113 74 74 68 58 60 68 70 66 68 60
130 110 106 96 103 117 110 104 106 102 104 102 79 69 70 63 71 79 73 74 68 65 71 69
110 90 84 95 88 96 101 111 107 100 102 68 66 60 58 58 64 71 66 69 72 68
122 107 90 86 100 106 104 108 106 103 100 102 100 70 74 66 64 68 72 69 76 68 70 76 68 72
122 120 125 117 111 112 106 103 100 88 116 69 75 81 76 81 71 88 71 56 42 75 145 146 134 138 142 121 127 102 119 130 94 94 82 87 88 80 81 60 76 79 120 110 106 100 90 88 126 138 80 76 69 70 62 70 86 76
100 91 84 93 99 95 92 92 92 67 67 62 60 63 61 62 60 63 121 106 97 104 102 90 106 110 109 112 72 70 66 67 70 64 67 73 70 74
109
MB
P -1
st min
MB
P –
2ndm
in
MB
P –3
rd m
in
MB
P- 4
th m
in
MB
P -5
th m
in
MB
P -6
th m
in
MB
P -7
th m
in
MB
P -8
th m
in
MB
P -9
th m
in
MB
P -1
0th m
in
MB
P -1
1th m
in
MB
P -1
2th m
in
MB
P -1
3th m
in
TVI
UA
B p
H
APG
SC
1
APG
SC5
PHE
USD
SID
TIM
E
94 89 79 76 81 84 83 86 81 90 7.2 9 10 200 480
98 94 87 78 78 83 83 87 90 88 88 110 7.2 10 10 200 540 96 91 86 79 76 83 83 86 85 90 7.2 9 10 200 480 90 87 80 72 73 70 79 82 84 90 7.18 10 10 300 480 93 85 78 81 79 82 84 87 84 87 89 87 120 7.18 9 10 100 600 89 85 71 71 75 82 83 86 86 83 82 110 7.12 9 10 200 540
98 92 87 79 77 82 77 83 78 85 85 110 7.15 9 10 400 600
97 92 84 81 77 80 83 85 85 85 100 7.16 8 10 300 540
97 94 87 83 78 72 80 85 88 84 83 86 120 7.13 8 10 200 600
95 89 73 69 71 74 78 78 81 81 100 7.19 9 10 200 480
93 86 81 77 75 79 80 83 83 80 82 110 7.2 10 10 300 540
95 82 73 73 83 81 83 75 82 81 100 7.18 9 9 200 540 88 81 78 75 73 76 76 81 79 90 7.15 9 10 100 480 85 80 73 69 66 70 79 84 85 83 100 7.2 9 10 400 540 87 84 72 68 69 72 75 77 80 79 100 7.17 9 10 400 540 84 79 70 71 82 81 70 76 82 82 81 83 120 7.18 9 9 200 600 93 92 79 69 73 81 87 79 81 78 100 7.18 8 10 200 480 96 83 82 74 82 92 85 84 81 77 82 80 120 7.2 9 10 100 600 82 74 68 70 68 75 81 81 82 81 79 110 7.18 10 10 300 600
87 85 74 71 79 83 81 87 81 81 84 79 81 130 7.18 10 10 200 600 87 90 96 90 91 85 94 82 71 57 89 110 7.21 8 9 100 540
111 111 99 104 106 94 96 74 90 96 100 7.18 9 9 100 480
93 87 81 80 71 76 99 97 80 7.11 10 10 200 360 78 75 69 71 75 72 72 71 73 87 90 7.15 9 9 100 480
88 82 76 79 81 73 80 85 83 87 100 7.21 10 10 200 540