Mandibulofacial Dysostosis
Transcript of Mandibulofacial Dysostosis

NOTES, CASES, INSTRUMENTS MANDIBULOFACIAL DYSOSTOSIS
R. P. THOMAS, M.D. Winston-Salem, North Carolina
Several recent case reports of mandibulofacial dysostosis,1-3 in the American literature indicate renewed interest in this syndrome. The case to be presented represents a transitional form between mandibulofacial dysostosis and craniofacial dysostosis.
The first reported case of mandibulofacial dysostosis is ascribed to Berry,4 in 1889, followed in 1900 by the report by Treacher Collins5 of the incomplete syndrome. Scattered reports subsequently appeared but it remained for Franceschetti6·7 and his group to delineate and define the syndrome in 1944 and 1949. The condition is also known by a confusing variety of eponyms (Collins-Franceschetti-Zwahlen syndrome, Franceschetti syndrome, and other combinations).
The complete syndrome consists of the following features (modified from Franceschetti and Klein7) :
1. Antimongoloid slant of the palpebral fissure.
2. Notching (coloboma) of the lower lids. 3. Hypoplasia of the facial bones, espe
cially the zygoma and the mandible. 4. Malformations of the external, middle,
and inner ear. 5. Macrostromia, high palate, and maloc-
clusion of the teeth. 6. Blind fistulas (dimples) between the
angles of the mouth and ears. 7. Atypical tongue-shaped processes of the
hair line extending toward the cheeks. 8. Other anomalies, especially skeletal de
formities. As with any syndrome, one or more fea
tures can be, and usually are, absent in any given case. The scarcity of reports on this condition attests to its rarity. The forme fruste may be indicated by notching of the lower lids, minimal hypoplasia of the facial bones or possibly by deformities of the ears.
These minimal signs may be more common than suspected.
That the syndrome is usually governed by an irregular dominant gene with variable expression is well documented. A number of cases, reported without family histories, may indicate mutations, or the operation of some environmental factor as yet unidentified. A search for possible environmental factors acting during the first trimester of pregnancy is worth while.
Mann8 attributes the defects to retarded differentiation of maxillary mesoderm involving the first visceral arch, occurring about the seventh fetal week. The notching of the lower lid is thought to represent the junction of paraxial and visceral mesoderm. This is thought to correspond to the junction of the area supplied by the first division of the trigeminal nerve with that area supplied by the second division. Little new material has been added to this classic description.
Although usually grouped with the cranio-stenoses, premature cranial synostosis is unusual. Oligophrenia associated with the syndrome has been noted, but appears to be the exception rather than the rule, in contrast to the true craniostenoses. It is speculative whether oligophrenia, when present, represents a developmental arrest or is secondarily a result of increased intracranial pressure. The latter is thought to be the usual cause of oligophrenia in the true craniostenoses. Odd-shaped skulls have been frequently associated with the syndrome, suggesting aberrant growth at the cranial sutures.
Vogt decried the idea of a separate name for every new combination of signs, and Howell9 re-emphasized this concept in his excellent review of the true craniostenoses. This viewpoint stresses the similarities of related syndromes rather than somewhat arbitrary and often ill-defined distinctions.
The interest of my case lies in the près-

NOTES, CASES, INSTRUMENTS 671
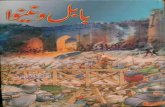
Fig. 1 (Thomas). Front view of patient.
Fig. 2 (Thomas). Side view of patient.
ence of several features usually associated with the true craniostenoses, and in particular with cranial-facial dysostosis (Crouzon's disease). These features are: (1) divergence of the orbital axes with resultant divergent squint, (2) shallow appearing orbits, and (3) apparent exophthalmos, in addition to features of mandibulofacial dysostosis. Straith10 previously described a case of mandibulofacial dysostosis with divergent strabismus. Divergence of the orbital axes is usually ascribed to lack of development of the greater wing of the sphenoid, which in normal development pushes the laterally directed fetal orbit to the forward directed adult position.
CASE REPORT
An 18-month-old girl was brought to the eye clinic for evaluation of a divergent strabismus. The infant was full-term. Birth weight, nine pounds, 11 ounces. The pregnancy was uneventful and no history of prenatal trauma or infections was elicited. The infant was noted to have a stridor during the neonatal period and has suffered recurrent upper respiratory infections. Examination of the mother and six siblings disclosed no visible or palpable stigmas of the syndrome. The father and three other siblings were said to be normal.
Physical examination revealed a well-nourished, alert white girl with odd facial features (figs. 1 and 2).
There was an antimongoloid slant of the palpe-bral fissures. A slight notch was noted in the lower lids approximately three mm. from the outer can-thus bilaterally. The inner portion of the lower lid appeared atrophie with a deficiency of lashes. There was a widely divergent strabismus, appearing to be the result of the divergent orbital axes. No individual muscle paralysis was elicited. The orbits appeared shallow, especially the right, and there was an apparent exophthalmos. Visual acuity appeared to be normal and the patient could alternate but preferred to use the left eye. The fundi appeared normal and no abnormalties of the disc were noted.
The pinnae of the ears were small, thickened and malformed. The external auditory meatus was absent on the right and stenotic on the left.
There was a palpable defect in the zygomatic arch, bilaterally, inferolateral to the orbits. The lower jaw was recessive, and there was a high arched palate. Prominent frontal bossing was noted. Deep dimples appeared on the cheeks with certain facial expressions. The birth record noted sinuses above each ear, but these have subsequently disappeared. The remainder of the physical examination was normal.
Radiologie examination demonstrated a fairly large defect in the zygomatic arch bilaterally and the body of the mandible was somewhat small.
North Carolina Baptist Hospitals Inc.
R E F E R E N C E S
1. Pavsek, E. J.: Mandibulofacial dysostosis. Am. J. Roentg., 79:598, 1958. 2. Seltzer, A. P.: The congenital defects known as Treacher Collins syndrome. EET Monthly, 37:396,
1958.

672 NOTES, CASES, INSTRUMENTS
3. Howard, J. L.: Mandibulofacial dysostosis (Franceschetti syndrome). Arch. Ophth., 59:882, 1958. 4. Berry, G. A.: Note on a congenital defect (coloboma) of the lower lid. Roy. London Ophth. Hosp.
Rep., 12:255, 1889. 5. Collins, E. T.: Case with symmetrical congenital notches in the outer part of each lower lid and
defective development of the malar bones. Tr. Ophth. Soc. U. Kingdom, 20:190, 1900. 6. Franceschetti, A., and Zwahlen, P.: Un syndrome nouveau: La dysostose mandibulo-faciale. Bull.
Schweiz Akad. med. Wiss., 1:60, 1944. 7. Franceschetti, A., and Klein, D.: The mandibulo-facial dysostosis: A new hereditary syndrome. Acta
Ophth., 27:143,1949. 8. Mann, I.: Deficiency of the malar bones with defect of the lower lids. Brit. J. Ophth., 27:13, 1943. 9. Howell, S. C : The craniostenoses. Am. J. Ophth., 37:359, 1954. 10. Straith, C. L., and Lewis, J. R.: Associated congenital defects of the ear, eyelids and malar bones
(Treacher Collins syndrome). Plastic & Reconst. Surg., 4:204, 1949.
M O D I F I C A T I O N O F A N O P H T H A L M O S C O P E *
FOR DIAGNOSIS OF FIXATION BEHAVIOR
G U N T E R K. VON NOORDEN, M.D. Iowa City, Iowa
The exact diagnosis of the fixation behavior in strabismic amblyopia is mandatory before treatment is initiated. This is important no matter whether one uses pie-optic methods or occlusion treatment alone. It has been pointed out1"3 that the conventional method of simple observation of the corneal light reflex on attempted monocular fixation is not a sufficiently accurate method to diagnose small fixation anomalies, such as parafoveal or paramacular fixation.
Two methods have been used by us in the past, allowing a more exact determination of the fixation behavior. Fixation photography4 is one method, but this method is generally confined to larger eye clinics where a fundus camera is available. The second instrumentation was introduced by Cuppers2
who developed the visuscope, a special ophthalmoscope with an asterisk inserted in the pathway of the light. The image of the asterisk is seen by the examiner on the fundus while the patient is invited to fixate the target. The mode of fixation can thus be readily recognized.
* From the Department of Ophthalmology, State University of Iowa Medical School.
The visuscope, however, may not be available in every office and, for exact and quick diagnosis of the fixation behavior, we have found a simple modification of the ordinary ophthalmoscope to be of excellent clinical value. This modification was described by Bangerter1 and can be readily applied to conventional ophthalmoscopes by any skillful optician.
Using a 1/4000 inch pivot watchmaker's drill, held with a pin vise, the interchangeable green filter of an ophthalmoscope is perforated in its center. A small bright dot in the center of the illuminated green field becomes visible to the patient, who is asked to fixate this target. The foveal reflex will be seen by the examiner within the brighter area when central fixation is present. Other retinal areas will appear in the center of the illuminated field in cases of non foveal fixation.
Care must be taken to reduce the brightness of the ophthalmoscope to some degree during the examination in order to maintain sufficient contrast between the darker surrounding and the brighter center, and thus provide an adequate fixation stimulus.
The technique of perforating the filter was suggested and carried out by Mr. Kenneth Hansen of the Iowa City Optic Company.
University Hospitals