Lbm 2 KGD SGD 8
-
Upload
sissi-komara -
Category
Documents
-
view
158 -
download
23
description
Transcript of Lbm 2 KGD SGD 8
Lbm 2 KGDSTEP 1 KETOPROFEN: obat anti inflamasi derivate dr asam profionat
STEP 21. Mengapa sesak nafas hebat setelah diberi suntikan ketoprofen?2. Apa hubungan riwayat sesak nafas berulang dan hipertensi sejak kecil dg gejala tersebut?3. Kenapa diberi suntikan adrenalin dan kortikostreroid serta diberi O2?4. Kenapa fase ekspirasi memanjang, wheezing, retraksi subcostal dan muka kebiru2an?5. Kenapa RR meningkat?6. Kenapa tekanan darah menurun?7. Kenapa nadi meningkat tp isi dan tegangan berkurang?8. Macam dosis pemberian oksigen?9. STEP 3Status Asthmaticus See Asthma REF: UpToDate 2006
Assessment| Management| Hospitalization|Useful algorithms| Recommendation
INTRODUCTION Severe attacks of asthma poorly responsive to adrenergic agents and associated with signs or symptoms of potential respiratory failure are often referred to as "status asthmaticus." The term is now applied toasthma attacks of unusual severity.
PATHOGENESISThe pathologic changes found on post-mortem examination of airwaysfrom most patients dying of severe asthma differ only in severity from those found in patients with mild asthma who die of other causes:1. Bronchial wall thickening from edema and inflammatory cell infiltration.2. Hypertrophy and hyperplasia of bronchial smooth muscle and submucosal glands.3. Deposition of collagen beneath the epithelial basement membrane.4. In addition, most asthma deaths are associated with prominent intraluminal inspissation of secretions, leading to occlusion of up to 50 percent of the total cross sectional area of airways two mm in diameter.5. In some deaths, however, bronchial mucus is absent, suggesting that airway obstruction was predominantly due to intense smooth muscle contraction.These pathologic patterns may correlate with differences in the rate of progression of attacks:1. A rapid response to bronchodilator therapy of "acute asphyxic asthma," in which the interval from the appearance of symptoms to intubation is less than three hours, has been interpreted as suggesting that bronchial smooth muscle contraction is the predominant cause of airway narrowing.2. The slower response to therapy of asthmatic exacerbations that progressed over many hours, days, or even weeks, may indicate greater contributions from mucus inspissation and inflammatory thickening of the bronchial wall.
Assessment| Management| Hospitalization|Useful algorithms| Recommendation
ASSESSMENT OF SEVERITYHistory The most powerful predictive feature in the history that a severe episode may be life-threatening is any history of prior intubation and mechanical ventilation for asthma. In comparison, progression of symptoms despite treatment with high doses of inhaled beta-agonists and oral or inhaled corticosteroids probably indicates a greater risk of a poor or slow response to initial emergency department therapy; it does not, however, alter recommendations for the initial therapy given.Physical examination Gross physical findings of severe asthma includeany alteration in consciousness, fatigue, upright posture, diaphoresis, and the use of accessory muscles of breathing. Tachypnea (>30/min), tachycardia (>120/min), and an inspiratory fall in systolic blood pressure (pulsus paradoxus) of more 15 mmHgare also more common in severe attacks. It is important to appreciate, however, that the absence of these findings does not exclude even immediately life-threatening airflow obstruction, especially if the patient is exhausted or obtunded.Examination of the chest typically revealsoverinflation, reduced respiratory excursion, and diffuse expiratory wheezing, but the pitch or intensity of wheezing does not discriminate between degrees of severity. Careful inspection of the mouth and pharynx and auscultation over the upper airway may provide clues that the site of obstruction is in the upper airway, as fromepiglottitis, angioedema, or vocal cord dysfunction.Measurement of peak expiratory flow rate The most direct assessment of airflow obstruction is measurement ofspirometry or peak expiratory flow rate (PEFR). However, some patients are too dyspneic to perform even this test until bronchodilator therapy has been given. Whenever possible, the PEFR should be measured initially to provide a baseline and at successive intervals during treatment. Predicted values differ with size and age, buta peak flow below 120 L/min or an FEV1 below 1.0 liters indicates severe obstruction for all but unusually small adults.Arterial blood gas measurements The most direct assessment of the impact of airflow obstruction on ventilation is measurement of arterial blood gases. The critical information lies not inarterial oxygen tension, for severe hypoxemia is rare in asthma and the customarily modest hypoxemia is responsive to modest oxygen supplementation. Far more important isthe arterial PCO2. Respiratory drive is almost invariably increased in acute asthma, resulting in hyperventilation and a correspondingly decreased PaCO2. Thus,an elevated or even normal PaCO2 indicates that airway narrowing is so severe that the ventilatory demands of the respiratory center cannot be met. Respiratory failure can then develop rapidly with any further bronchoconstriction or respiratory muscle fatigue. BecauseCO2 retentiondevelops only in severe asthma and oxygen saturation can be measured by pulse oximetry, arterial blood gases need not be measured in most asthmatic patients presenting for emergency care. Furthermore, even patients with CO2 retention usually respond to aggressive drug therapy, so it could be argued thatarterial blood gases need only be determined on initial assessment in the following cases: Patients gasping for air. Patients unable to speak more than two or three words. Patients with obtunded consciousness or in cardiopulmonary arrest. Patients with severe asthma who respond poorly to initial aggressive therapy. Repeated evaluation after initial treatment may be even more important than the initial assessment of severity. The response to the first two hours of treatment appears to be the most powerful predictor of outcome.
Assessment| Management| Hospitalization|Useful algorithms| Recommendation
Management of Status Asthmaticus *Correction of any precipitating causes!1. Oxygen supplement2. Bronchodilatorsa.Inhaled Beta agonistsasalbuterol (Ventolin/Proventil)- It is most commonly given by handheld nebulizer, at a dose of2.5 mg dissolved in two mL of isotonic saline.- In patients with particularly severe obstruction, nebulized albuterol may be given continuously until the obstruction is improved or toxicity (tachycardia, arrhythmias, skeletal muscle tremor) supervenes.- The modestfall in the plasma potassiumconcentration of about 0.7 meq/L caused by intensive beta-agonist therapy may induce slight Q-T prolongation on the electrocardiogram. However, this translocation of potassium into the cells is infrequently of practical importance except for patients who are hypokalemic from other causes or who are taking digitalis. Similar modest falls in the plasma magnesium and phosphate concentration also occur via the same mechanism.
b.Ipratropium bromide (Atrovent)by inhalation- As a practical matter, it appears that the addition of0.25 mg of ipratropium to a large dose of albuterol (five mg) in the solution given by nebulizerresults in greater improvement in FEV1 than does albuterol alone (26 versus 20 percent in one study)- For patients requiring frequent bronchodilator aerosol treatment for several hours, alternating albuterol and ipratropium treatments offers a way of maintaining bronchodilation while reducing the risk of beta agonist toxicity.
c.Theophyllineby intravenous infusion adds to the bronchodilation achieved by maximal doses of an inhaled beta agonist.- Most short-term studies show that intravenous infusion of theophylline (aminophylline) adds toxicity but no further immediate bronchodilation to that achieved by nebulized therapy with a beta agonist. Furthermore, most longer-term studies show that addition of intravenous theophylline to inhaled beta agonist and intravenous corticosteroid therapy has no influence on the course or duration of hospitalization 3. Corticosteroids- dramatically reduces the need for hospitalization and should be instituted in patients who do not respond immediately to bronchodilators.- reducing mucosal edema and inflammatory cell infiltration; and decreasing mucus secretion- for example,IV methylprednisolone (125 mg)given on presentation to the emergency department was associated with a hospitalization rate of 19 percent compared to 47 percent in the placebo treated group.- the current practice ofmethylprednisolone 2 mg/kg IV q6hr. However, a meta-analysis of 30 randomized trials suggests that half that dose is probably maximally effective.-PO 60 mg of prednisone q6hrappears to as effective as intravenous methylprednisolone. Once oral corticosteroids are started, they should be continued for at least one week, and the patient should be seen in follow-up before the dose is tapered or discontinued. It was once common practice to reduce the dose gradually, such as a decrease of five mg of prednisone every other day over seven to ten days. However, there appears to be little risk in abruptly stopping short courses (ie, less than 10 days) of oral therapy in patients whose symptoms, physical findings, and peak flow have normalized.- both40 mg and 125 mg of methylprednisolone IV q6hrcaused a significantly more rapid improvement in FEV1 than did 15 mg.- Inhaled corticosteroids may take several days for their effects to become apparent, and possibly several months before they reach a plateau [49]. As a result, inhaled therapy should be started before oral therapy is discontinued. 4. Parenteral magnesium The two largest prospective, double blind, controlled studies reported thus far showed that magnesium sulfate added little or no further bronchodilation to that achieved with an inhaled beta agonist. However, the numbers of subjects studied were too few to definitely exclude possibly responsive subgroups, such as premenopausal women._ The dose of magnesium typically given,2 gm IV over 20 minutes, has little toxicity and is unlikely to harm a patient with severe asthma. Nevertheless, we cannot recommend magnesium sulfate until there is evidence that at least some patients benefit from its addition to usual therapy. 5. Antibiotics Viral but not bacterial respiratory infections are common precipitants of asthma exacerbations. It is therefore not surprising that amoxicillin has been shown not to affect the course of acute asthmatic attacks. Antibiotics are now reserved for patients with fever, leukocytosis (>15,000/mm3), and a pulmonary infiltrate on the chest radiograph. 6. Intubation & Ventilator-The decision to proceed to intubation and mechanical ventilationshould be made before the patient is in extremis. Asthmatics have exaggerated bronchial responsiveness, and intubation is difficult in any circumstance, let alone under the conditions of hypoxia, hypercapnia, and acidosis of respiratory failure. There are no explicit and inclusive guidelines as to when intubation should be performed; the decision to proceed is best based on an integrative clinical assessment of the patient's ability to continue ventilation until therapy becomes effective.Worsening fatigue and persistent or increased hypercapnia weigh heavily in favor of intubation.The initial goal of therapy is simply to reverse obstruction to airflow, as documented by improvement in the peak flow or FEV1 obtained 1 to 2 hours after therapy is started. The ultimate goal is a sustained improvement in either measurement to >70 percent of predicted or the patient's personal best. This should be accompanied by a decrease in symptoms, so that the patient is no longer short of breath at rest or with minimal exertion
Hospital Management of Asthma Exacerbation
1. Mengapa sesak nafas hebat setelah diberi suntikan ketoprofen?Ketoprofen= antiinflamasi Efek samping: hipersensitivitasmediator inflamasibronkokonstriksiobstruksi pertukaran o2 terganggu hipoventilasisesak nafasInflamasipermeabilitas meningkatedemsesak nafas (anafilaktiktipe 3)Pertukaran O2 terganggu co2 lebih tinggi alkalosis respiratorikhipoksemia terlalu lama asidosis metbolikMediator inflamasitdk ada kontraksi otot pernafasan peningkatan permeab dan kebocoran vaskuler edem sesak nafas
Kaltrofen adalah obat yang mengandung ketoprofen dan termasuk dalam golongan obat anti inflamasi non steroid (AINS), derivat asam propionat. Obat anti inflamasi non steroid merupakan obat yang mempunyai efek analgesik (penghilang rasa sakit), antipiretik (penurun panas) dan antiinflamasi (menghilangkan pembengkakan).
Seperti obat golongan AINS lain, maka Kaltrofen juga mempunyai efek analgesik, antipiretik dan juga antiinflamasi. Mekanisme kerjanya adalah dengan cara menghambat sintesa prostaglandin, yang merupakan suatu zat yang dapat menyebabkan inflamasi.
Kaltrofen diindikasikan untuk menekan berbagai reaksi inflamasi yang dihubungkan dengan nyeri dan demam. Seperti pada penyakit sendi (rematoid artritis dan osteoartritis), penyakit gigi dan mulut, paska bedah, paska trauma dan paska persalinan.efek samping dari ketoprofen adalah bronkospasme. selain itu, kontraindikasi juga org yg hipersensitifitas thd ketoprofen. sehingga dapat memacu reaksi sesak nafas.
INDIKASI KONTRAINDIKASI KETOPROFEN?PT Kalbe Farma memproduksi 4 macam sediaan kaltrofen, yaitu :1. Tablet regular release 50 mg dan 100 mg, yang diberikan 3 kali sehari.Tablet sustained release 200 mg, yang diberikan 1 kali sehari.2. Suppositoria 100 mg, yang diberikan 1-2 kali sehari.3. Injeksi 100 mg/2 ml4. Topikal, jelli 30 gram (0,025 gram ketoprofen/gram).Berbagai bentuk sediaan tersebut dapat digunakan sesuai dengan kebutuhan. Sediaan tablet sustain release akan lebih nyaman digunakan karena cukup 1 kali minum perhari. Selain itu juga telah disediakan bentuk gel yang lebih praktis dalam pemakaiannya. Bentuk sediaan topikal dapat digunakan untuk :1. Trauma ringan, seperti trauma yang disebabkan oleh cedera olah raga, terkilir, pembengkakan.2. Nyeri paska trauma.Indikasi: Untuk mengobati gejala-gejala artritis rematoid, ankilosing spondilitis, gout akut dan osteoartritis serta kontrol nyeri dan inflamasi akibat operasi ortopedik.Kontraindikasi: Hipersensitif terhadap ketoprofen, aspirin dan AINS lain Gangguan fungsi ginjal dan hati yang berat
EFEK SAMPING KETOPROFEN? Mual, muntah, diare, dyspepsia, konstipasi, pusing, sakit kepala, ulkus peptikum hemoragi perforasi, kemerahan kulit, gangguan fungsi ginjal dan hati, nyeri abdomen, konfusi ringan, vertigo, oedema, insomnia. Reaksi hematologi : trombositopenia. Bronkospasma dan anafilaksis jarang terjadi.
MEKANISME KERJA KETOPROFEN?Ketoprofen merupakan suatu antiinflamasi non steroid dengan efek antiinflamasi, analgesik dan antipiretik. Sebagai anti inflamasi bekerja dengan menghambat sintesa prostaglandin. Pada pemberian oral kadar puncak dicapai selama 0,52 jam. Waktu paruh eliminasi pada orang dewasa 3 jam, dan 5 jam pada orang tua.interaksi obat: Pemakaian bersama dengan warfarin, sulfonilurea atau hidantoin dapat memperpanjang waktu protrombin dan perdarahan gastrointestinal. Pemakaian bersama dengan metotreksat dilaporkan menimbulkan interaksi berbahaya, mungkin dengan menghambat sekresi tubular dari metotreksat.
2. Apa hubungan riwayat sesak nafas berulang dan hipertensi sejak kecil dg gejala tersebut?Hipersensitifitasmediator inflamasidlm darah vasokontriksi berlebihhipertensiSesak nafas krn alergi (alergen2 tertentu)Hipersensitif asma bronchial yg menghubunkan cincin2 tulang rawan mengkerut memendek berkontraksi prod lendir berlebih ditambah infeksi pembengkakanHipertensitek darah meningkat resistensi pemompaan darah oleh jantung terjadi beban jantung menambahkompensasihipertrofi ventrikel kiri keleahan ventrikel dan pembuluh darah kebutuhan o2 meningkt jk tidak terpenuhi hipoksisesak nafas
3. Kenapa diberi suntikan adrenalin dan kortikostreroid serta diberi O2?Adrenalin broknospasme Kortikosteroid inflamasi, mencegah kebocoran mikrovaskuler, Cara kerja= menghambat metab asam arakidonat mempngaruhi prod prostaglandin, leukotrient Mengurangi kebocoran mikrovaskuler Menghambat prod sitokin Mencegah migrasi langsung sel2 inflamasiDiberikan setelah adrenalin tidak berefek
Hipoksi O2 Untuk mempertahankan tekanan o2 (70-80mmHg) untuk mengurangi beban pernafasan
4. Kenapa fase ekspirasi memanjang, wheezing, retraksi subcostal dan muka kebiru2an?Penyumbatan bronkus, penebalan lap ukus, sumbatan lumen--. Resistensi intratorakal meningkat inspirasi bisa ekspirasi susah fase ekspirasi memanjang tenaga berlebih wheezingRetraksi subkostal krn dadanya sulit mengembangkompensasi mencari o2 lbh banyakMuka Kebiruanhipoksiperfusi o2 jaringan kurang5g hb yang tidak berikatan dg o2
PATOGENESIS RETRAKSI SUBCOSTAL, WHEAZING, NAFAS CUPING HIDUNG, MUKA KEBIRUAN, DAN FASE EKSPIRASI MEMANJANG?Keluhan utama penderita asma ialah sesak napas mendadak, disertai fase inspirasi yang lebih pendek dibandingkan dengan fase ekspirasi, dan diikuti bunyi mengi (wheezing), batuk yang disertai serangn napas yang kumat-kumatan. Pada beberapa penderita asma, keluhan tersebut dapat ringan, sedang atau berat dan sesak napas penderita timbul mendadak, dirasakan makin lama makin meningkat atau tiba-tiba menjadi lebih berat.Wheezing terutama terdengar saat ekspirasi. Berat ringannya wheezing tergantung cepat atau lambatnya aliran udara yang keluar masuk paru. Bila dijumpai obstruksi ringan atau kelelahan otot pernapasan, wheezing akan terdengar lebih lemah atau tidak terdengar sama sekali. Batuk hamper selalu ada, bahkan seringkali diikuti dengan dahak putih berbuih. Selain itu, makin kental dahak, maka keluhan sesak akan semakin berat.Dalam keadaan sesak napas hebat, penderita lebih menyukai posisi duduk membungkuk dengan kedua telapak tangan memegang kedua lutut. Posisi ini didapati juga pada pasien dengan Chronic Obstructive Pulmonary Disease (COPD). Tanda lain yang menyertai sesak napas adalah pernapasan cuping hidung yang sesuai dengan irama pernapasan. Frekuensi pernapasan terlihat meningkat (takipneu), otot Bantu pernapasan ikut aktif, dan penderita tampak gelisah. Pada fase permulaan, sesak napas akan diikuti dengan penurunan PaO2 dan PaCO2, tetapi pH normal atau sedikit naik. Hipoventilasi yang terjadi kemudian akan memperberat sesak napas, karena menyebabkan penurunan PaO2 dan pH serta meningkatkan PaCO2 darah. Selain itu, terjadi kenaikan tekanan darah dan denyut nadi sampai 110-130/menit, karena peningkatan konsentrasi katekolamin dalam darah akibat respons hipoksemia.Wheezing pada saat ekspirasi :Pada asma, diameter bronkiolus lebih berkurang selama ekspirasi daripadaselama inspirasi karena peningkatan tekanan dalam paru selama eksirasi paksamenekan bagian luar bronkiolus. Karena bronkiolus sudah tersumbat sebagian,maka sumbatan selanjutnya adalah akibat dari tekanan eksternal yangmenimbulkan obstruksi berat terutama selama ekspirasi. Pada penderita asmabiasanya dapat melakukan inspirasi dengan baik dan adekuat, tetapi sekali-kalimelakukan ekspirasi. Hal ini menyebabkan dispnea. Kapasitas residu fungsionaldan volume residu paru menjadi sangat meningkat selama serangan asma akibatkesukaran mengeluarkan udara ekspirasi dari paru. Hal ini bisa menyebabkanbarrel chest. (Tanjung, 2003)
5. Kenapa RR meningkat?Kompensasi untuk mencari o2 lebih banyak
6. Kenapa tekanan darah menurun?Kompensasi jantungEfek obat krn pelepasan mediator inflamasi(bradikinin) vasodilatasi tekanan darah menurunMediator inflamasiPermeabilitas meningkatvaokonstriksiPermeabilitas meningkatkebocoran vaskuler volume intravaskuler menuruntekanan darah menurunTek darah menurun krn syok anafilaktik krn kegagalan sirkulasi dan respirasiSyok cardiogenik tek darah systole < 90mmhg, diskenario 90/60 mmhg, sudah termasuk syok/blum??Proses anafilaktik??Terapi tekanan systole < 90mmhg??
Pulsus paradoxus is a particular well known example of the interaction between the heart and lungs during spontaneous breathing seen with either wide swings in pleural pressure, a patient with status asthmaticus with excellent respiratory muscle reserve being an example of this, or cardiac tamponade related to inadequate filling of first the right and subsequently the left side of the heart related to external compression of the cardiac chambers. We recognize that pulsus paradoxus is exaggerated by hypovolemia. The physiology that I will now describe has sometimes been referred to as reverse pulsus paradoxus because it occurs during the opposite phase of the ventilatory cycle from pulsus paradoxus in patients who are being ventilated with positive pressure. Figure 1 illustrates the physiology for stroke volume variation during positive pressure ventilation.
Figure 1In Figure 1, we see displayed in the top panel the airway pressure from four positive pressure breaths simultaneously displayed with the arterial waveform directly below it. It is easy to follow the swings in blood pressure and their timing to the ventilatory cycle by looking at these two tracings together. Blood pressure goes up during the inspiratory phase of mechanical ventilation and decreases during expiration. When we see this at the bedside in a patient who is hypotensive, we know intuitively that they will respond to volume. Interestingly and importantly, those patients who dont respond to volume actually inform us about their peculiar physiology and may lead to specific diagnoses, i.e. cardiac tamponade (more on this later).As the ventilator cycles, there is an acute increase in intrathoracic pressure. We are familiar primarily with the dramatic impact that this may have on right ventricular filling and function. This also sets the stage for the swings in stroke volume and consequently blood pressure that we are familiar with during positive pressure ventilation. RV afterload is increased simply by the mechanical pressure of the individual alveoli on the pulmonary capillaries. The right ventricle sees that as increased afterload (Figure 2).
Figure 2 shows the impact of alveolar inflation on RV afterload and LA fillingRV right ventricle; LA left atrium; Pa pulmonary arteriole; Pv pulmonary vein; PA AlveolusSimultaneously RV preload is decreased due to a smaller gradient for venous return when the chest is pressurized. Simply, the driving force for venous return (which equals cardiac output) can be simply defined as the pressure difference between intrathoracic and extrathoracic vessels. As the intrathoracic pressure increases, this pressure gradient for venous return is decreased, and therefore less blood will flow into the right side of the heart during the inspiratory phase of positive pressure ventilation. Approximately 3-5 cardiac cycles later, this smaller volume ejected by the right ventricle shows up on the left side of the heart and then in the systemic circulation as decreased stroke volume and cardiac output. This is the predominant effect of positive pressure ventilation on both stroke volume and blood pressure and is well known. Perhaps less well appreciated is the acute augmentation in stroke volume during the inspiratory phase of positive pressure ventilation. This affect at the alveolar capillary interface can simply be thought of as the alveolus inflating, compressing the adjacent pulmonary vein, and that displaced blood volume moving to the left side of the heart (Figure 2).This acute augmentation in left ventricular preload, the right side of the diagram in Figure 1, causes an acute increase in stroke volume and consequently blood pressure during the inspiratory phase of positive pressure ventilation. This describes the basic, but perhaps not simple, physiology.In studying Figure 1, it should become apparent that changes in the breathing pattern or in pleural pressure on a breath-to-breath basis would impact stroke volume variation dramatically. Similarly, changes in the RR interval seen on EKG or felt in the pulse would also dramatically impact stroke volume variation independent of the physiology I have just described. Furthermore, it is important to recognize, and I think we intuitively understand, that stroke volume variation is significantly impacted by the volume status of the patient. Thus, the linear relationship between stroke volume variation and preload responsiveness. The greater the stroke volume variation, the greater the response to a volume challenge. (Figure 3)
Figure 3: Multiple Starling curves represent individual patients or a single patient whose cardiac performance varies throughout the course of illness and treatment. Determining where a patient is on their own Starling curve at any point in their illness is what makes this data pair SVV:SV a major breakthrough in our ability to care for the critically ill. When SVV is elevated (>13% - A), patients are on the preload dependent part of the curve and will respond to volume. B represents the preload independent portion of he curve and if cardiac performance (SV) is inadequate, therapy other than volume is necessary to augment cardiac performance.If filling of the ventricles is changing on a beat-to-beat interval because of a significant dysrhythmia, and atrial fibrillation is the best example of this, there is significant variation in stroke volume simply related to the variability in filling time caused by the irregular rhythm that will not reflect volume responsiveness. Simply, there can be tremendous stroke volume and pulse pressure variability with a significant dysrythmia that is related to the rhythm problem itself and not volume status. In these instances, stroke volume variation or pulse pressure variation tells us nothing about volume responsiveness or the patients position on the Frank-Starling curve. Similarly, albeit through a different mechanism, an irregular breathing pattern, i.e. spontaneous breathing commonly, where both the tidal volume and the cycle length from breath to breath vary, may also induce stroke volume variation that is not related to volume responsiveness. The more irregular the breathing pattern and depth of ventilation is, at least potentially the more exaggerated this problem becomes. This is further complicated by insufficient pleural pressure change in spontaneously breathing patients to meaningfully impact venous return. The use of dynamic variables for volume responsiveness has not and will not be validated generally in spontaneously breathing patients for these reasons.The question then becomes what to do with these patients to ascertain whether or not they are volume responsive. Fortunately, the answer is simple and intuitive as long as we have the ability to measure a change in stroke volume. This represents a huge advantage of the technologies that allow measurement of stroke volume and cardiac output, namely FloTrac/Vigileo, PICCO, and LIDCO, over those that simply provide pulse pressure variation, which is now easily available on bedside monitors that display an arterial waveform. This physiology also explains why the bulk of this literature has been developed in the operating room where the ideal conditions often exist for the measurement and application of dynamic parameters, namely controlled mechanical ventilation with a large enough tidal volume to induce a significant change in pleural pressure to impact venous return. Indeed, a threshold value for tidal volume of 8 cc per kilogram ideal body weight has been determined in several studies that evaluated this specific question, the concept being that below this threshold value of 8 cc/kg, there is not enough pleural pressure change to meaningfully impact venous return. Across a heterogeneous population, this may indeed be true, although there will be specific examples depending on the patients lung compliance and intravascular volume status where it may not be. At lower tidal volumes, you may get some false negatives, for lack of a better term, where stroke volume variation is low, but the patient may still be significantly volume responsive. The converse is unlikely to be true. If at a lower tidal volume, there is significant variability in stroke volume, generally those patients would be expected to be volume responsive. We encountered extreme examples of this during the H1N1 flu epidemic in the fall of 2009, where many of our patients were being oscillated at very high frequencies but with minimal tidal volume and hence pleural pressure change. These patients could be significantly volume responsive with essentially no stroke volume or pulse pressure variation because of the imperceptible change in pleural pressure with this strategy of ventilation. Similarly, patients being ventilated using a low tidal volume strategy may manifest a similar phenomenon. In those patients, teasing out volume responsiveness utilizing physiology is fairly simple. What we do in my Intensive Care Unit for these patients is one of three things:1. We acutely increase the tidal volume to at least 8 10 cc/kg and look for the change in stroke volume variation. For volume responsive patients, once we go beyond the threshold value for tidal volume, often this becomes apparent in stroke volume variation, it will increase to greater than 13%. The time responsiveness of these technologies is fairly rapid and tidal volume needs to be increased for only a short period of time, less than 5 minutes with the FloTrac/Vigileo system and often 2 minutes is enough to show significant change. We will also stand at the bedside during this maneuver to a) view the change; and b) assure that the pressures encountered with the ventilation change are not harmful to the patient.2. Another strategy that has been proven to be extremely effective in this regard is the passive leg raising maneuver (PLR). The patient is laying flat and the legs are elevated to 45 degrees (Figure 4).
Figure 4(Those patients in whom stroke volume variation becomes greater than 13% are then given a fluid bolus typically after being returned to the initial ventilator settings with the tidal volume approach, or returned to their prior position in bed after the PLR maneuver and the change in stroke volume and cardiac output is recorded. This can be done numerous times until the indicator of volume responsiveness disappears or an adequate stroke volume/cardiac output is reached.) The legs need to be elevated for roughly 120 seconds using the FloTrac/Vigileo system and a similar time for the PICCO system to assess what the increase in venous return from this gravitational maneuver induces in cardiac performance. Those patients that have a positive response usually defined as greater than 12-15% increase in cardiac output are then given a fluid challenge. In numerous studies, this has been shown to be essentially a perfect test as a measure of volume responsiveness as long as the improvement in stroke volume/cardiac output is the cardiac performance parameter of interest. This technique works well especially in those patients who are either spontaneously breathing or have a significant dysrhythmia. This reversible volume challenge ismost usefulin patients with acute lung injury or ARDS or those with either acute or chronic renal failure, where giving a volume challenge that does not result in improvement in cardiac performance may in fact be detrimental to the patient.1. As long as there is a cardiac performance measure, again stroke volume or cardiac output, simply giving a fluid bolus and assessing its impact on cardiac performance is a reasonable way to go in those patients in whom we suspect that additional volume will not be injurious, i.e. clear lungs or without renal failure. If cardiac performance does not improve, volume is not the answer. When beginning to utilize these technologies, it is not uncommon to have to prove this to yourself several times, i.e. giving multiple fluid challenges and seeing no improvement in cardiac performance, but this is all part of the learning curve with new technologies.At some point, however, it is important to recognize that the patient is on the flat part of the Frank-Starling Curve andnotresponding to volume (Figure 3), as ultimately excess volume has been associated with increased length of stay, increased time on mechanical ventilation, and mortality. The major impact of using these technologies well is that we now have the ability for precise titration of volume management in the majority of critically ill patients. A simple premise to consider as I close is why do we give volume or attempt volume challenges in the critically ill in any circumstance. My strong contention is the only reason we do this is to affect a change in cardiac performance, thus begging the question on how are we able to do this intelligently, using physiology, without a cardiac performance measure?May , 2011 - Blog # 1 - Dr. McGee on HemodynamicsWilliam T. McGee, M.D., MHA, FCCP is Associate Professor of Medicine and Surgery at Tufts University School of Medicine, Boston, Massachusetts. His interests are in ARDS, vascular access (pulmonary artery catheterization), sepsis, nutrition, and nosocomial pneumonia. He has published > 67 papers, chapters and abstracts. He is the principal investigator for clinical trials studying the efficacy and safety of rfPAF-AH for the prevention of ARDS in patients with severe sepsis. He is a three-time recipient of Excellence in Teaching Award from Tufts University School of Medicine, the Society of Critical Care Medicine Internal Medicine Specialty Award for Influence of Insurance Status on Pulmonary Artery Catheter Use and The Presidential Citation Award from the Society of Critical Care Medicine for outstanding contribution to the Society during 1999. He is a Director for the Fundamentals of Critical Care Support Course for the Society of Critical Care Medicine. He is on the review board for the Journal of Intensive Care Medicine.
7. Kenapa nadi meningkat tp isi dan tegangan berkurang?Kompensasi jantung syok anafilaktik Macam2 syok??
8. Macam dosis pemberian oksigen?
9. Perbedaan sesak nafas cardia dan pulmonal serta penatalaksanaan?Cardia pd >40th,tiba2, krn stress/capekAkibat kongesti jantungsesak nafas cardiaPulmonal dr muda, pelan2, krn Krn asma
BEDA SESAK NAFAS DARI PARU DAN DARI JANTUNG?Kalau ciri-ciri sesak nafas karena penyakit jantung sbb :1. Ada tekanan yg berat menimpa dada sebelah kiri2. Nyeri seperti ditusuk didada sebalah kiri3. Lemas dan mata berkunang-kunangKalau ciri-ciri sesak nafas karena asma sbb:1. Sesak seluruh dada baik kiri maupun kanan2. Tidak dapat bernafas lancar3. Kepala pusingJANTUNGhipertensi kerja jantung makin berat kardiomegali dekompensasi kordis gangguan fungsi pompa jantung gangguan fungsi pompa darah dari [paru penumpukan darah pada organ paru peningkatan tekanan pada pembuluh darah paru fungsi paru terganggu sesak nafas sesak nafas timbul saat melakukan aktivitas berat aktivitas ringan sesak nafas terasa saat menghela nafas perlu posisi duduk agar nafas terasa lebih ringan serangan jantung korornersesak nafas diawali nyeri dada yg khas seperti tertindih beban berat pada dada sisi kiri menjalar ke leher, lengan kiri, pundak, punggung, dan mgkn sampai muntah2.==> hanya bersifat serangan kardiomegali keluhan sesak nafas sudah dimulai sejak awal.ASMA sesak nafas terasa saat ekspirasi sesak nafas terasa lebih ringan jika duduk mendekap bantal atau merangkul sandaran kursi ada wheazing
10. Sesak Napas Definisi dan mencangkup tanda dan gejalaKesulitan bernapas , terlihat adanya kontraksi dari otot-otot pernapasan tambahan yang ditandai dengan tambahan jumlah frekuensi napas dan juga ada napas cuping hidung, disertai dengan gelisah . Etiologi Obstruksi saluran nafas ( benda asing , alergi ) Ketidakseimbangan sistem saraf otonom Oedem pulmonal Gagal jantung kiri Penyakit paru Pnemuthorak Efusi pleura Tension pneumothorak PPOK Psikis Paralisis otot-otot pernafasan pada SGB dan MIAS STEMIA GRAVIS
PatofisiologiObstruksi saluran nafas : Alergi : Atopik : adanya hipersensifitas tipe 1 ( diperentarai IgE dan mediatornta adalah histamin ) terjadinya sangat cepat Tahap sensitasi Degranulasi ( histamin , serotonin dan bradikinin ) spasme , peningkatan permeabilitas pembuluh darah , sekresi mukus yang berlebih penyempitan saluran napas Non atopik ( H Tipe 3 , IgG dan IgM , terjadi kompleks imun, )Reaksinya timbul 4-6 jam Atopik dan Non atopik ( campuran )Keadaan : ( bronkokontriksi , hipersekresi mukus , oedem bronkus , inflamasi bronkus )Ketidakseimbangan otonom : antara kolinergik dan adrenelgik ?? ( adit ) Klasifikasi berdasarkan Derajat 0 : normal 1 : ada kesulitan bernapas saat berjalan ditempat landai 2 : berjalan labih lambat 3: berhenti jalan untuk bernapas 4 : terlalu sulit untuk bernapas saat melakukan kegiatan yg ringan Penatalaksanaan dan efek sampingnya ( dosis ) ?? Sesak napas : Bronkodilator , Kortikosteroid , pemberian oksigen ,
Berdasarkan penyebabnya, asma bronkhial dapat diklasifikasikan menjadi 3 tipe,yaitu :1. Ekstrinsik (alergik)Ditandai dengan reaksi alergik yang disebabkan oleh faktor-faktor pencetus yangspesifik, seperti debu, serbuk bunga, bulu binatang, obat-obatan (antibiotic danaspirin) dan spora jamur. Asma ekstrinsik sering dihubungkan dengan adanyasuatu predisposisi genetik terhadap alergi. Oleh karena itu jika ada faktor-faktorpencetus spesifik seperti yang disebutkan di atas, maka akan terjadi seranganasma ekstrinsik.2. Intrinsik (non alergik)Ditandai dengan adanya reaksi non alergi yang bereaksi terhadap pencetus yangtidak spesifik atau tidak diketahui, seperti udara dingin atau bisa juga disebabkanoleh adanya infeksi saluran pernafasan dan emosi. Serangan asma ini menjadilebih berat dan sering sejalan dengan berlalunya waktu dan dapat berkembangmenjadi bronkhitis kronik dan emfisema. Beberapa pasien akan mengalami asmagabungan.3. Asma gabunganBentuk asma yang paling umum. Asma ini mempunyai karakteristik dari bentukalergik dan non-alergik.Perisai Husada - Klinik Spesialis Penyakit Dalam & Saraf
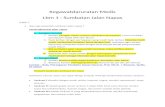
Pembagian asma bronchial menurut beratnya serangan akut :
RingansedangBeratGagal nafas mengacam
SesakBerjalanDapat berbaringLebih suka dudukMembungkuk kedepan
Cara bicaraBeberapa kalimatSatu kalimatkata
KesadaranMungkin gelisahUmumnya gelisahgelisahMengantuk atau bingung
Frekuensi napasMeningkatMeningkat>30menit
Retraksi otot bantu nafasBiasanya tidak adaBiasanya adaadaGerakan paradoksal torakoabdominal
MengiRingan- sedangKeraskerasmenghilang
APE % terhadap standar (sesudah terapi)>70-80%50-70%